by Martin Furmanski MD
Scientist’s Working Group on Chemical and Biologic Weapons
Center for Arms Control and Nonproliferation
February 17, 2014
NOTICE: THIS WORK MAY BE PROTECTED BY COPYRIGHT
YOU ARE REQUIRED TO READ THE COPYRIGHT NOTICE AT THIS LINK BEFORE YOU READ THE FOLLOWING WORK, THAT IS AVAILABLE SOLELY FOR PRIVATE STUDY, SCHOLARSHIP OR RESEARCH PURSUANT TO 17 U.S.C. SECTION 107 AND 108. IN THE EVENT THAT THE LIBRARY DETERMINES THAT UNLAWFUL COPYING OF THIS WORK HAS OCCURRED, THE LIBRARY HAS THE RIGHT TO BLOCK THE I.P. ADDRESS AT WHICH THE UNLAWFUL COPYING APPEARED TO HAVE OCCURRED. THANK YOU FOR RESPECTING THE RIGHTS OF COPYRIGHT OWNERS.
Introduction
The danger to world or regional public health from the escape from microbiology laboratories of pathogens capable of causing pandemics, or Potentially Pandemic Pathogens (PPPs) has been the subject of considerable discussion1,2,3,4 including mathematical modeling of the probability and impact of such escapes5. The risk of such releases has generally been determined from estimates of laboratory infections that are often incomplete, except for the recent 2013 Centers for Disease Control (CDC) report6, which is a significant source of recent data on escapes from undetected and unreported laboratory-acquired infections (LAIs).
This paper presents an historical review of outbreaks of PPPs or similarly transmissible pathogens that occurred from presumably well-funded and supervised nationally supported laboratories. It should be emphasized that these examples are only the “tip of the iceberg” because they represent laboratory accidents that have actually caused illness outside of the laboratory in the general public environment. The list of laboratory workers who have contracted potentially contagious infections in microbiology labs but did not start community outbreaks is much, much longer. The examples here are not “near misses;” these escapes caused real-world outbreaks.
Methods of pathogen identification
Modern genetic analysis allows pathogens to be identified, and given a sufficient catalog of isolates of the same pathogen, it is possible to determine if two specimens are identical or very closely related. Because all pathogens that are circulating in the environment show genetic changes over time, one can date the time the pathogen circulated. For instance, for 20th century human and swine influenza viruses beginning in the 1930s, one can generally place a virus to a particular year. With modern rapid genomic analysis outbreaks can be traced with considerable accuracy: for instance the 2009 pandemic pH1N1 influenza outbreak has been analyzed with confidence limits of branchpoints in its first wave defined within days or weeks, and individual transmission chains can be identified7.
Example #1: British smallpox escapes, 1966, 1972, 1978
The WHO’s successful effort to eradicate natural transmission of smallpox in the 1970s highlighted the risk that virology laboratories posed as a source of epidemics. This was clearly demonstrated in the United Kingdom, where from 1963-1978 only 4 cases of smallpox (with no deaths) were reported from smallpox endemic areas, while during the same period at least 80 cases and 3 deaths were the result of three separate escapes of the smallpox virus from two different accredited smallpox laboratories.8 Much of the current policy and practice in biosafety and biocontainment of dangerous pathogens can be traced to the political and professional reaction to these outbreaks.
The UK became a sensitive test system for smallpox laboratory escapes because it ended compulsory smallpox vaccination in 1946. Public sentiment in the UK had always included significant resistance to and apathy towards vaccination, and so by the mid 1960s and through the 1970s a large proportion of children and young adults had never been vaccinated, and many older persons were never re-vaccinated after initial childhood or military vaccinations. Thus the protective herd immunity in the general public, which earlier rendered impotent any laboratory escapes, disappeared. At the same time, the considerable volume of travel and immigration from smallpox endemic areas of Africa and the Indian subcontinent meant that surveillance for imported smallpox cases was required. UK maintained several smallpox laboratories at medical schools for both research and to support clinical diagnosis.
The first laboratory outbreak to be recognized began in March 1972, in a 23 year old laboratory assistant at the London School of Hygiene and Tropical Medicine, who had observed harvesting of live smallpox virus from eggs. This had been done on an open bench, as was routine, the laboratory having no isolation cabinets at that time. Before she was placed in isolation, she infected two visitors to a patient in an adjacent bed, both of whom died. They in turn infected a nurse, who survived9.
The recognition of this laboratory escape resulted in several investigations, which led to the establishment of guidelines for laboratories handling smallpox and other dangerous pathogens. These recommendations included handling dangerous pathogens in biological safety cabinets only in certain dedicated rooms by specifically trained and designated personnel. Also guidelines were issued for isolation with dedicated gowns and gloves, and the establishment of proper ventilation facilities to maintain negative pressure in these rooms and cabinets. These recommendations are the direct precursors to the current Biosafety Laboratory (BSL) level protocols.
By 1977 the natural chain of smallpox transmission had been interrupted, and the WHO was in the process of reducing the number of laboratories holding smallpox virus. In August of 1978 a 40 year old medical photographer at Birmingham Medical School developed smallpox, and died. She infected her mother, who survived. She worked in a studio and darkroom that was immediately above the smallpox laboratory at Birmingham Medical School. Investigation revealed that although the long established laboratory had been inspected and approved to handle smallpox virus, it did not have sufficient facilities to meet the new biocontainment requirements, and was scheduled to be decommissioned at the end of 1978. Moreover, work on smallpox had accelerated substantially in order to complete existing projects before the closing, and work with smallpox was performed by laboratory personnel who did not receive appropriate training and supervision, and appropriate isolation practices were frequently violated. The most likely route of exposure of the Medical Photographer was by transport of infectious aerosols generated by a centrifuge through building ventilation ducts that were improperly sealed and allowed aerosols to be delivered to one of the Photographer’s working spaces. Laboratory notebooks and the photographer’s work logs indicated that the strain infecting the photographer was handled in the laboratory on the same days that the photographer worked in the potentially contaminated workspace, on dates consistent with the photographer’s calculated exposure date. Dr Henry Bedson, a world renowned smallpox investigator who was responsible for the Birmingham laboratory, committed suicide as a result of the outbreak (Shooter 1980).
The 1978 investigation re-examined a 1966 smallpox outbreak, which in retrospect was strikingly similar to the 1978 outbreak. The earliest case identified in 1966 was in a medical photographer who worked at Birmingham Medical School in the same facility as the 1978 case. This outbreak was caused by a low-virulence strain of smallpox (variola minor), and it caused at least 72 cases of smallpox from February to August 1966, spread through the midlands of Britain, and Wales. The vast majority of cases were in unvaccinated children or young adults. There were no deaths. Retrospective review again revealed variola minor had been manipulated in the smallpox laboratory at a time appropriate to cause the infection in the photographer working a floor above.
Example #2: The “re-emergence” of H1N1 human influenza in 1977.
Human influenza H1N1 viruses appeared with the 1918 pandemic, and persisted, slowing accumulating small changes in its genome (with a major change in 1947), until the H2N2 “Asian” flu appeared in 1957, causing a worldwide pandemic. H1N1 influenza virus then apparently became extinct, and was not isolated for 20 years. In 1969 the “Hong Kong” H3N2 virus replaced the H2N2 virus, and is still circulating.
In September 1977 an H1N1 influenza virus was isolated from human infections in the Far East region of the Soviet Union, and in early 1978 the Chinese reported they had isolated H1N1 virus in May of 1977 in northeast China adjacent to the Soviet outbreak1011. Using the early genetic tools available at the time, the 1977 H1N1 virus was found to be closely related to H1N1 human influenza viruses circulating in 1949-1950, but not to those circulating earlier or later12, 13.
The 1977 H1N1 flu virus rapidly spread worldwide, in a pandemic that was restricted largely to people under ~ 21 years of age. Older persons had been exposed to related H1N1 viruses prior to 1957, and carried substantial immunity. Mercifully, the “re-emergent” H1N1 virus was not very virulent. Although illness was widespread, affecting 20-70% of those under 20 years of age in school or military camp outbreaks in the first year14, deaths were few. Many asymptomatic infections were detected by serology (Kung 1978).
The appearance of this “time-traveling throwback” puzzled virologists, because no similar examples had previously been identified in influenza or other similar viruses. Initially escape of a virus kept in storage from c1950 from a virology lab was discussed, but such a laboratory accident was denied by Chinese and Soviet virologists (Kung 1978, Beveridge 1978). Western virologists quietly let the matter of a laboratory escape origin for the 1977 H1N1 virus drop from discussion, out of an abundance of scientific caution, and also out of an eagerness not to offend the Russian and Chinese scientists, whose early gestures of cooperation in worldwide influenza surveillance system were very important to foster, because such cooperation would allow tracking influenza globally.
Discussions of the origins of the 1977 H1N1 gave rise to hypotheses of natural “biological stasis” or viral latency in an undefined animal. Experimental investigations of possible transmission of human H1N1 viruses in avians were pursued, but with minimal success and no demonstration of persistent avian transmission15, nor were human viruses identified in avians in very extensive subsequent surveys. The ambiguous term “frozen evolution” was coined, allowing for the freezing to be biologically functional, metaphorical, refrigerative, or natural.
A 2006 paper16 claimed to have isolated H1N1 influenza virus RNA from ice and meltwater from Siberian lakes that were frequented by migratory birds. Since migratory birds naturally carry and shed a wide variety of influenza viruses, and since year to year variations in the amount of thawing of lake ice might allow influenza viruses shed from the migratory birds to remain physically frozen for a number of years, the paper stated this might be the mechanism for the re-emergence of the 1977 H1N1 flu. It emphasized the 1977 H1N1 link because the RNA sequences it reported isolating from the lakes were closely related to sequences of three H1N1 reference viruses that it characterized as being of avian origin that circulated in the late 1960s.
Problems soon arose with this paper, however. The authors issued a correction17 in 2007 indicating the H1N1 reference strains originally characterized as avian and from the 1960s were in fact of human origin, and dated from the 1930s. A paper highly critical of the 2006 Siberian Lake paper was published in 2008 18, presenting strong evidence that the reported isolation of influenza RNA from nature was the result of contamination in the laboratory by the standard reference strain of human H1N1 virus (isolated in 1933) that was used as a positive control in that laboratory.
Presently, with detailed sophisticated genomic analysis available, and with 32 years of circulation of the 1977 H1N1 virus available for study, no evidence of natural genomic stasis has been identified. It has become clear that its appearance in 1977 was almost certainly due to escape from a virology lab of a virus sample that had been frozen since c1950. Only since 2008 have virologists actually begun to make the suggestion of a probable laboratory release in scientific papers: “The reemergence in 1977 is unexplained and probably represents reintroduction to humans from a laboratory source19,” and “…little A/H1N1 evolution is evident over the twenty-year period of the virus’s global disappearance, supporting earlier suggestions that this subtype was most likely accidentally reintroduced into human circulation from a laboratory environment20.” It should be noted that this paper calculates the 1977 H1N1 virus had been circulating for 1 year before it was reported, so that geographic origin cannot be stated with certainty.
Only since 2009-2010 did major papers begin to state directly the 1977 emergence of H1N1 influenza was a laboratory related release: “The most famous case of a released laboratory strain is the re-emergent H1N1 influenza A virus which was first observed in China in May of 1977 and in Russia shortly thereafter21.” The paper made this statement in part because the continued “agnostic” approach to the 1977 re-emergence introduced unacceptable errors in calculating the genomic divergence dates for influenza virus strains.
Public awareness of the 1977 H1N1 pandemic and its likely laboratory origins has been virtually absent. Virologists and public health officials with the appropriate sophistication were quickly aware that a laboratory release was the most likely origin, but they were content not to publicize this, aware that such embarrassing allegations would likely end the then nascent cooperation of Russian and Chinese virologists, which was vital to worldwide influenza surveillance. An abundance of caution in making such suggestions was also in their own self-interest. The 1976 “swine flu” alarm and subsequent immunization program that proved to be unneeded caused 532 cases of Guillain-Barre syndrome and 32 deaths. It was widely considered a misadventure, and had severely damaged the public and political credibility of the virology and public health communities. An acknowledgement of a pandemic originating from their laboratories would have only worsened it. The most plausible reason for a Chinese or Russian laboratory to thaw out and begin growing a c1950 H1N1 virus in 1976-77 was as a response to the US 1976 “swine flu” program, which resulted in a program to immunize the entire US population against H1N1 influenza virus. It was clearly a rational response for other countries with virology capabilities to explore making their own H1N1 vaccines. Thawing available frozen stocks of virus was necessary, because H1N1 was no longer circulating. Modern commentators have begun to articulate this connection between the 1976 Swine flu immunization program and the 1977 H1N1 re-emergence:
“Perhaps an even more serious consequence [of the 1976 swine flu episode] was the accidental release of human-adapted influenza A (H1N1) virus from a research study, with subsequent resurrection and global spread of this previously extinct virus, leading to what could be regarded as a ‘self-fulfilling prophecy’ epidemic.” (Zimmer 2009)
The speculation that the 1977 release may have been related to H1N1 vaccine research is supported by the observation that in the initial outbreaks in China, nine of the ten viral isolates expressed “temperature sensitivity” (Kung 1978). Temperature sensitivity normally an uncommon trait, but one that was in the 1970s (and still is) a fundamental trait for making live attenuated influenza vaccines. Temperature sensitivity generally occurs only after a series of substantial laboratory manipulations and selections. Interestingly, further investigation indicated the circulating strains in 1977-78 were often comprised of mixed temperature-sensitive and normal components, and that temperature sensitivity apparently disappeared from the post-1978 H1N1 lineage rapidly22. Escape of a mid-protocol population of H1N1 virus undergoing laboratory selection for temperature sensitive mutants would provide such a mixed population. In 1976-77 laboratory personnel in their late teens or early 20s would not have been exposed to pre-1957 H1N1 influenza viruses, and been susceptible to laboratory infections. The low severity of the 1977 pandemic might be in part due to the temperature sensitivity of the virus, a trait that limits virus replication in pulmonary tissues.
Example #3 Venezuelan Equine Encephalitis in 1995
Venezuelan Equine Encephalitis (VEE) is a viral disease transmitted by mosquitoes that intermittently erupts in regional or continental-scale outbreaks in the Western Hemisphere that involve equines (horses, donkeys and mules), termed epizootics, and often with concurrent epidemics among humans. The disease in equines creates high fever and severe neurological symptoms (colloquially termed “pesta loca” [crazy plague] in Spanish, or “blind staggers” in English) and a high, 19-83% fatality rate. In humans symptoms can vary from asymptomatic to a mild influenza-like febrile illness to a severe acute incapacitating febrile illness often with neurological symptoms (headache, depression, incoordination, mental clouding, epileptic seizures). Though its severity varies between outbreaks, VEE in humans may be fatal (up to ~5%) or, particularly in children, leave permanent neurological disability (epilepsy, paralysis, mental retardation) in 4 to 14% of clinical cases. In humans and equines miscarriages and stillbirths are increased.
Outbreaks typically occur in South America, though the 1969-71 continental-scale epizootic/epidemic reached from Central America through Mexico to Texas. VEE viruses are classified by their surface antigens, with the types causing large scale epizootics and epidemics being classed as type IAB and IC (termed epizootic strains), and types causing only sporadic human or equine disease in localized areas falling into types ID, IE, IF and II through VI (termed enzootic strains).
With modern genomic investigations available since the mid 1990s, programs of surveillance of mosquitoes and wildlife in regions at risk have discovered that in nature the enzootic VEE viruses are maintained by continuous transmission by mosquitoes in small mammals in the tropical and subtropical western hemisphere. The epizootic/epidemic type IAB and IC viruses appear suddenly without evidence of ongoing transmission during the long intervals between major outbreaks23. Moreover, genomic studies indicate that the epizootic types of VEE originate from the enzootic strains, specifically strain ID having given rise to the epizootic/epidemic types IAB and IC through a process of mutation24. VEE virus, like influenza virus shows rapid spontaneous changes in its genome, so that one can determine not only the genetic relatedness but also quantify the chronological distance separating different viral strains.
This is where the elegance of modern viral genomics becomes an embarrassment to virologists. It is clear from the genomics that while the enzootic type ID VEE virus can indeed mutate into the epizootic/epidemic types IAB and IC, it has, in fact, only done this on three occasions: ID to IAB some time in the 1930s and ID to IC in 1963 and 1992. There had been significant outbreaks of VEE every few years from the 1930s to the 1970s, however, and analysis showed that the numerous type IAB outbreaks were essentially matches to the original 1938 IAB VEE isolation that had been used in veterinary vaccines since the late 1930s. The veterinary vaccines had used inactivated (i.e. “killed”) whole virulent viruses. VEE is notoriously hard to inactivate in the lab, and laboratory infections were common. It was clear that many batches of the veterinary VEE vaccines had not been completely inactivated, in which residual infective virus remained.
From 1938 to 1972, the VEE vaccine was causing most of the very outbreaks that it was called upon to control, a vicious cycle indeed, and another example of “self-fulfilling prophecy” outbreaks.
The recognition that inadequately inactivated vaccines caused most VEE outbreaks caused a change in the veterinary vaccine seed virus to an attenuated strain, and VEE outbreaks apparently ceased for 20 years, from 1973 to 1992 25. Then, in 1992 a VEE outbreak in Venezuela occurred which proved to be a IC virus that was shown by genomic studies to have spontaneously arisen from enzootic type ID viruses circulating in the area where it arose, much like what had also occurred in the same area of Venezuela in 1962-64, when ID had mutated to a IC and caused an outbreak. The two IC VEE viruses, from 1962-64 and 1992, were distinct from each other, and arose from different genetic lines of ID viruses. The mystery of how epizootic VEE viruses arise naturally was apparently solved.
However, in 1995 a major VEE epizootic and epidemic hit Venezuela and Colombia, with a type IC virus also the cause. There were at least 10,000 human VEE cases with 11 deaths in Venezuela26 and an estimated 75,000 human cases in Colombia, with 3,000 neurological complications and 300 deaths27. Household attack rates ran 13-57% and VEE virus was isolated from 10 stillborn or miscarried human fetuses28.
Full genomic studies identified the 1995 virus as identical to an 1963 isolate with no sign that this virus had been circulating and the acquiring small genetic mutations indicative of replicating in hosts for 28 years. It was another case of “frozen evolution.” But it could not be another case of an outbreak caused by a defective inactivated VEE vaccine, because the 1963 type IC VEE virus had never been used to make a vaccine. Possible trans-ovarian transmission in mosquito vectors had been explored previously with negative results29. Suspicion fell on an inadvertent release from a virology lab, either by an unrecognized infection of a lab worker or visitor, or escape of an infected laboratory animal or mosquito. VEE is easily transmitted by the aerosol route during laboratory manipulations, and laboratory infections with VEE are common in unvaccinated persons. In this outbreak there was considerable circumstantial evidence for such a laboratory escape. The 1963 type IC VEE virus was used in an “inactivated” form as a reagent for testing purposes, and this reagent preparation was tested and was found to contain live virus. This reagent was used in the virology laboratory in Venezuela located where the 1995 outbreak first appeared, which was in an area without ongoing circulation of type ID enzootic viruses related to the 1963/1995 IC virus, and an area removed from where de novo IC VEE outbreaks had previously originated. Moreover, a report from this lab of an IC virus isolated from a surveillance mosquito pool in 1983 proved to be identical to the IC antigen strain, indicating a previous laboratory contamination event. The major scientific group working on VEE published a paper in 2001 stating the outbreak most likely was a laboratory escape, though this could not be proven30.
The situation becomes less clear-cut, because in 2005 the same group reported small outbreaks from 2000 and 2003 with multiple isolations of IC virus from equids in Venezuela, this time one identical to the 1995 virus31. Yet another example of “frozen evolution” but during a period when the 1963/1995 IC virus was no longer used widely as a reagent preparation, and it originated in an area with ongoing enzootic transmission of VEE viruses. The VEE working group backed off its earlier conclusion that the 1995 outbreak was likely laboratory mediated, but was unable to propose a natural process for the genomic stasis they reported.
The VEE working group clearly has great expertise, and one must respect their judgment that the 2000 isolations are valid and laboratory circumstances are significantly different than in 1995, so that natural genomic stasis may indeed exist for VEE and is worthy of further investigation. Several proposed mechanisms for genomic stasis for VEE have been proposed and investigated. VEE circulates in a complex ecological pattern, with enzootic transmission involving a variety of mosquito and mammalian hosts, so various theories allowing genomic stasis have been proposed, such as latency in an arthropod line or mammalian host. These have been investigated with multi-year surveys in enzootic and post-epizootic areas, and no definite evidence of persistent epizootic strains have been found in arthropods or small mammals. In addition to the negative surveys, the short lifespans of small mammals and of the potential arthropod hosts preclude viral latency from explaining the 5 or 28 year hiatuses in the appearances of the “frozen” IC epizootic viruses, and no evidence has been found for latency in the longer-lived human and equine hosts. Transovarian “vertical” propagation of viruses in arthropods between mother and progeny has been described with some pathogens in arthropods, and this has been investigated experimentally with VEE in VEE vectors, without positive results32.
It is clear that laboratory strains of VEE virus have a decades-long established habit of re-appearing showing “frozen evolution,” and causing “self-fulfilling prophecy” epidemics. It is clear that escape of laboratory strains of this virus through faulty vaccines has occurred multiple times in the past. Strong circumstantial evidence exists for an inadvertent escape in 1995, and a re-emergence in 2000 is without explanation.
Example 4: SARS laboratory escapes outbreaks after the SARS epidemic
The SARS outbreak of 2002-2003 eventually spread to 29 countries, causing over 8,000 infections and at least 774 deaths. Because many cases were in hospital workers (1707, amounting to 21%), it had the potential to shut down health care services where it struck33. By imposing strict (sometimes draconian) quarantines on exposed persons and isolation of patients, and even more because of good fortune and dedicated (indeed, heroic) medical personnel, it was contained and extinguished by July 2003. Quarantines, closure of factories and travel restrictions caused economic losses estimated at $40 billion worldwide, with an estimated 2.6% GDP loss in China, 1.05% GDP loss in Hong Kong, and 0.15% GDP loss to Canada34.
SARS is particularly dangerous to handle in the laboratory because there is no vaccine, so all laboratory workers are susceptible. It can be transmitted through aerosol/droplet mechanisms: the very large (321 cases) Amoy Gardens outbreak in Hong Kong was traced to infectious aerosols created by turbulent flushing water flow in the sewer lines: this turbulent flow generated aerosols that were sucked back up into numerous adjacent apartments through dry floor drains by negative pressure generated by bathroom exhaust fans! (Abraham 2005).
Moreover, about 5% of SARS patients are “super-spreaders” who pass the infection to many (over 8) secondary cases35. One case (ZZ) spread SARS to directly to 28 persons during one 18-hour hospitalization, before transfer to another hospital, where he infected 93 additional hospital personnel. At a third hospital he infected 23 staff and 19 patients, and at a fourth 20 hospital staff (Abraham 2005). Another super-spreader in Beijing infected at least 59 secondary cases. A super-spreader originally infected by ZZ in China visited Hong Kong but fell ill and remained in his hotel room, but managed to spread SARS to 10 secondary cases whose only associations were using a common elevator or hallway. These Hong Kong hotel exposures were international tourists, however, and were responsible for spreading SARS to Canada, Ireland, the US, Singapore, and Vietnam36. A 72-year old was already ill when he boarded flight CA112 from Hong Kong to Beijing on March 15, after having visited a niece ill with SARS in a Hong Kong hospital. Besides introducing another transmission chain in Beijing, on the two-hour flight he infected 20 other passengers and 2 flight attendants, who spread the disease to Mongolia, Singapore, Taiwan, and re-introduced new infection chains back into Hong Kong37 (Abraham 2005).
The existence of SARS “super-spreaders” makes even a single laboratory infection into a potential pandemic.
SARS has not naturally recurred, but there have been six separate “escapes” from virology labs studying it: one each in Singapore and Taiwan, and in four distinct events at the same laboratory in Beijing.
The first escape was in Singapore in August 2003, in a 27-year-old virology graduate student at the National University of Singapore. He had not worked directly with SARS, but SARS was present in the virology laboratory where he worked with West Nile Virus (WNV). Investigation showed that his preparation of WNV was contaminated with SARS virus, and that this was the likely origin of his infection. After falling ill on Aug 26, he sought outpatient medical care in several venues, and was admitted to the hospital only on September 3. Fortunately he recovered and there were no secondary cases. Investigation revealed multiple shortcomings in infrastructure, training and observed procedures at the laboratory, and remedial actions were ordered38.
The second escape was in Taiwan in December 2003, when a SARS research scientist fell ill on a return airflight after attending a medical meeting in Singapore Dec 7-10. Although he felt his illness was SARS, he remained at home for 5 days, unwilling to seek medical care because he dreaded bringing disgrace to himself and his institution. He was only persuaded to enter the hospital when his father threatened to commit suicide39. Preliminary investigation implicated a laboratory exposure due to an attempt to decontaminate a bag of leaking biological waste, perhaps without proper protection and against protocol the day before he left for Singapore40. His 74 contacts in Singapore were put under quarantine for ten days, but again, fortunately none developed SARS. An expert committee from WHO investigated the laboratory and its procedures, and recommended improvements41.
This second outbreak further shook the virology communities in Asia, where many labs held and worked on SARS samples. On December 18, 2003 WHO released a new protocol for handling SARS specimens in the post-outbreak period, with special emphasis on reducing risk of and performing surveillance to detect laboratory infections42. Although this protocol was clearly created after the first (Singapore) escape, WHO chose to parse its words to avoid offending members. Perhaps distinguishing between a primary laboratory infection and secondary spread into a community “outbreak,” it chose to treat the risk as hypothetical, stating in the introduction:
“The possibility that a SARS outbreak could occur following a laboratory accident is a risk of considerable importance, given the relatively large number of laboratories currently conducting research using the SARS-CoV or retaining specimens from SARS patients. These laboratories currently represent the greatest threat for renewed SARS-CoV transmission through accidental exposure associated with breaches in laboratory biosafety.”
The hypothetical outbreak was not long in coming.
On April 22, 2004 China reported a suspected case of SARS in a 20-year-old nurse who fell ill April 5 in Beijing. The next day it reported she had nursed a 26-year-old female laboratory researcher who had fallen ill on March 25. Still ill, the researcher had traveled by train to her home in Anhui province where she was nursed by her mother, a physician, who fell ill on April 8 and died April 19. The researcher had worked at the Chinese National Institute of Virology (NIV) in Beijing, which is part of China’s Center for Disease Control (CDC), and which was a major center of SARS research. The investigation at NIV also uncovered an unrelated laboratory infection in a 31-year old male laboratory researcher at the NIV who fell ill on 17 April [43]. The entire NIV institute was closed and all of its 200 employees placed in quarantine in a hotel. Subsequent investigation confirmed these first three cases as SARS, and eventually identified a total of nine cases, in three generations, including health care workers and their family contacts44. Neither of the two primary patients had worked with live SARS virus, and WHO investigators had “serious concerns” regarding biosafety procedures at the NIV45.
Several Chinese and international groups investigated the outbreak at the NIV, and identified in retrospect two additional SARS laboratory infections at the NIV that had previously gone unrecognized and had begun in February 2004 [46]. A joint China CDC and WHO investigation found many shortcomings in biosecurity at the NIV, and traced the specific cause of the outbreak to an inadequately inactivated preparation of SARS virus that was used in general (not biosecure) laboratory areas in the NIV, including the one in which the two primary cases worked. It had not been tested to confirm its safety after inactivation, as it should have been. The WHO also found more general shortcomings in the handling of live SARS virus and a lack of surveillance of laboratory personnel for laboratory infections.
Li Liming, director of the China CDC and his deputy directory, the director of the NIV and his deputy director, and the director of the division where the two index cases worked were removed from their positions and found guilty of negligence in overseeing safety at the institution47. The Chinese government also decided to move the China CDC campus from its position in a residential neighborhood to an area “more remote from downtown,” and to allocate funds for more advanced laboratory equipment and infrastructure48.
Interestingly, the virology community is still reticent to discuss laboratory escapes: despite the considerable alarm these escapes created in the public health community and the participation of US CDC personnel in their investigation, they go unmentioned in the “10 years after” historical review of SARS by the CDC.49
Example 5: Foot and Mouth Disease (FMD) from Pirbright 2007
Foot and Mouth Disease (FMD) is a veterinary disease that affects primarily cloven-hoofed domestic animals (pigs, sheep and cattle). It has been eradicated in North America and most of Europe. It is highly transmissible, capable of spreading through direct contact and even through some prepared meats (sausages, airline food), on boots of farm workers (or tourists’ shoes: that’s why there’s that question “have you visited a farm” on the re-entry customs checklist coming into the USA), and even by aerosol spread.
FMD only occasionally causes a mild disease in humans, though exposed humans can carry the virus for up to three days, potentially an important method of spread. FMD causes a more serious disease in animals. Often fatal in young animals, survivors are stunted and lose their economic value. Adult animals die less often, but fail to gain weight or drop in milk production, and can become carriers. Most importantly, strict international quarantine regulations mean that an outbreak will cause all livestock and meat from that country to be banned from international trade. Various methods of outbreak control exist, but all are draconian, requiring massive culling (killing) of “in contact” but otherwise healthy animals surrounding index cases. Restrictions on all animal movement and often all commerce through infected areas are imposed, resulting in secondary economic losses from loss of tourism and general economic activity.
For instance, in the UK in 2001 a FMD outbreak ran from February to October 2001, with travel and export restrictions lasting into 2002. To control the outbreak, all susceptible livestock within 3 kms of an active case were culled. At its peak, 80,000-93,000 animals a week were killed and burned on farms, a total about 10 million sheep and cattle. Its direct cost was about $6.9 billion with overall costs to the British economy estimated at $16 billion.
On August 3, 2007 an outbreak of FMD was reported on a farm in the UK, initially with at least 38 cases in cattle identified. Quarantine measures were introduced and an investigation begun, with culling of surrounding livestock. Most countries banned UK livestock and meat exports. The virus was quickly identified as a strain that had caused a 1967 outbreak in the UK, but was not currently circulating in animals anywhere. Another case of “frozen evolution.” However, this outbreak was 2.8 miles (4.6 kms) south of Pirbright, where the only two facilities in the UK that were authorized to hold FMD virus were located. One was the UK Institute for Animal Health (IAH), the other Merial, a commercial veterinary FMD vaccine manufacturer. They both used the 1967 FMD strain, the Merial facility in large amounts (10,000 l) for vaccine manufacture. Operations were suspended at Merial on August 4 and its license to operate withdrawn. A second FMD outbreak quickly appeared near the first, and animal movement with the UK restricted and quarantine zones encompassing both the Pirbright campus and two affected farms were put in place on Aug 750. An initial investigation also published August 7 found no evidence for aerosol or surface water transmission of FMD virus from Pirbright, was investigating other wastewater issues, and suggested human carriage might have occurred51.
Investigation eventually showed that a waste-water line carrying partially treated waste water from the Merial vaccine plant to the final waste treatment plant run by IAH had gone without routine inspection or maintenance, was damaged, leaking, and had an unsealed manhole opening to the surface, so was capable of contaminating ground and surface water. It became clear that Merial and the IAH each considered the other responsible for such inspection and maintenance, and it had gone undone. The non-secure wastewater line ran through a construction area that recent heavy rains had turned into deep mud, and construction vehicles traversed it and exited the Pirbright campus without inspection or monitoring. These trucks sometimes used the road that passed by the first affected farm. It was concluded that contaminated mud from the defective wastewater line at Pirbright had been carried on tyres or underbody of construction vehicles and caused the first outbreak52.
For a brief time the outbreak was thought to have ended, and restrictions in the Pirbright area were lifted September 8, 2007. The UK applied to the EU to lift most restrictions on animal exports from the UK to EU on September 11, 2007.
However, on September 12, 2007 FMD was again reported, this time 30 miles north of Pirbright, again with the same 1967 strain of FMD. From September 18-30 multiple additional outbreaks of FMD appeared in the same area. A national embargo on all animal shipment was imposed, and new surveillance zones expanded rapidly until, overlapping they encompassed a portion of Heathrow Airport and were cut across by the major M4, M3 and M25 motorways. Rapid (real-time) genomic analysis had been ongoing during this outbreak, and indicated a single escape of FMD from Pirbright, which first spread between the two farms of the August outbreak, then went unnoticed at third farm before it blossomed again in mid September. Follow-up investigations identified the intermediate farm53.
The 2007 UK FMD outbreak identified 278 infected animals, and required 1578 animals to be culled54. It disrupted UK agricultural production and exports, and cost an estimated 200 million pounds. The ban of meat exports was particularly damaging as UK beef had only just exited a 10-year embargo by the EU because of BSE (Mad Cow Disease) in May of 2006.
FMD is such an easily transmitted virus with such potential to cause massive economic damage it would appear that manipulating it in a virology laboratory in a FMD free area is manifestly fraught with hazard. Particularly when it might escape by an “invisible” breach in biosafety as it did at Pirbright, and where it might lurk undetected despite heavy surveillance as it did between the two outbreaks.
In the US, previous law had banned it on the continental US, so FMD virus is currently only held in the USDA Plum Island facility off of Long Island (in a facility originally built in the 1950s for anti-animal BW [biological weapons] work). Currently a replacement facility under the Department of Homeland Security (DHS), the National Bio-and Agro-Defense Facility (NBAF) is under construction in Manhattan, KS. The move of FMD research to the agricultural heartland of the US was opposed by many groups, including the GAO, but DHS decided on the KS location and construction is ongoing. So much for learning from other’s experience.
Conclusions
There are some common themes in these narratives of escaped pathogens. Undetected flaws in the functioning of what was considered at the time to be an adequate standard of technical biocontainment is one theme, as demonstrated in the UK smallpox and FMD cases. Transfer to and handling of inadequately inactivated preparations of dangerous pathogens in areas of the laboratory with reduced biosecurity levels (allowable if the preparation is actually inactivated) is another theme, demonstrated in the SARS and VEE escapes. Poor training of personnel and slack oversight of laboratory procedures negated policy efforts by national and international bodies to achieve biosecurity in the SARS and UK smallpox escapes. The recent appearance of a cohort of immunologically naïve people in the general population, which previously had been uniformly immune was a factor in the UK smallpox and the 1977 H1N1 escapes; in this regard it should be remembered that there is no immunity at all in the general population to most potentially pandemic pathogens currently under discussion, such as Avian influenza and SARS.
It is hardly reassuring that despite stepwise technical improvements in containment facilities and increased policy demands for biosecurity procedures in the handling of dangerous pathogens, that escapes of these pathogens regularly occur and cause outbreaks in the general environment. Looking at the problem pragmatically, question is not if such escapes will happen in the future, but rather what the pathogen may be and how such an escape will be contained, if indeed it can be contained at all.
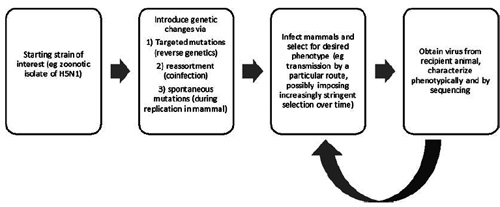
Advances in genetic manipulation now allow the augmentation of virulence and transmissibility in dangerous pathogens, and such experiments have been funded and performed, notably in the H5N1 avian influenza virus. The advisability of performing such experiments at all, and particularly in laboratories placed at universities in heavily populated urban areas, where laboratory personnel who are potentially exposed are in daily contact with a multitude of susceptible and unaware citizens is clearly in question.
If such manipulations should be allowed at all, it would seem prudent to conduct them in isolated laboratories where personnel are sequestered from the general public and must undergo a period of “exit quarantine” before re-entering civilian life55. Such isolated “detached duty”, while inconvenient for the lifestyle of virologists, is hardly foreign to them, since many experience prolonged periods of inconvenient and dangerous field work in the collection of viruses in the field, and certainly many other natural scientists do prolonged and isolated field work as well. The “inconvenience” barrier that requiring such isolation may present to principal investigators and other personnel may act as a natural screening factor to insure that dangerous manipulations to dangerous pathogens are only undertaken when genuinely indicated.
_______________
REFERENCES
1 Marc Lipsitch and Barry R. Bloom 2012. Rethinking Biosafety in Research on Potential Pandemic Pathogens . mBio 3(5): . doi:10.1128/mBio.00360-12.
2 Klotz, LC. The Human Fatality and Economic Burden of a Man-made Influenza Pandemic: A Risk Assessment. Unpublished Jan 2014. May be accessed at http://armscontrolcenter.org/The_Human_ ... 1-5-14.pdf or http://bio-security.org/wp-content/uplo ... 1-5-14.pdf
3 Merler S, Ajelli M, Fumanelli L, and Vespignani A. Containing the accidental laboratory escape of potential pandemic influenza viruses. BMC Medicine 2013, 11:252 doi:10.1186/1741-7015-11-252 http://www.biomedcentral.com/1741-7015/11/252
4 Scientists call for urgent talks on mutant-flu research in Europe. By Heidi Ledford. Nature 20 December 2013 http://www.nature.com/polopoly_fs/7.145 ... letter.pdf
5 Klotz LC, Sylvester EJ. The unacceptable risks of a man-made pandemic. Bulletin of the Atomic Scientists 7 Aug 2012.
6 Henkel R, Miller T, and Weyant RS. Monitoring Select Agent Theft, Loss and Release Reports in the United States—2004-2010. Applied Biosafety 17 (4) 2012 http://www.absa.org/abj/abj/121704FAHenkel.pdf Escaped Viruses-final 2-17-14
7 Baillie GJ, et al. Evolutionary dynamics of local Pandemic H1N1/2009 Influenza virus lineages revealed by whole-genome analysis. J Virol 86(1):11-18 Jan 2012.
8 Shooter RA. Report of the Investigation into the Cause of the 1978 Birmingham Smallpox Occurrence. HMSO 1980. Available: http://www.official-documents.gov.uk/do ... 8/0668.pdf
9 Fenner F. Henderson D. A. Et al. Smallpox and its Eradication. Published by World Health Organization, Geneva, 1988. ISBN 10: 9241561106 / ISBN 13: 9789241561105 available online: http://apps.who.int/iris/handle/10665/39485.
10 Kung HC, et al. Influenza in China in 1978: recurrence of influenza virus A subtype H1N1. Bull WHO 56(6):913-918 (1978).
11 Beveridge WIB. Where did red flu come from? New Sci. 1978 Mar 23;77/1095:790–1.
12 Nakajima K, Desselberger U, Palese P. Recent human influenza A (H1N1) viruses are closely related genetically to strains isolated in 1950. Nature. 1978;274:334–339.
13 Scholtissek C, von Hoyningen V, Rott R. Genetic relatedness between the new 1977 epidemic strains (H1N1) of influenza and human influenza strains isolated between 1947 and 1957 (H1N1). Virology. 1978;89:613–617
14 Chakraverty P. The return of the historic influenza A H1N1 virus and its impact on the population of the United Kingdom. J Hyg, Camb (1982) 89: 89-100
15 Shortridge KF. Et al. Reappearance of H1N1 influenza virus in man: evidence for the persistence of the virus in domestic chickens. Bull WHO 57(3):475-477 (1979)
16 Zhang G, Shoham D, Gilichinsky D, Davydov S, Castello JD, Rogers SO. Evidence of influenza a virus RNA in siberian lake ice. J Virol. 2006 Dec;80(24):12229-35. Epub 2006 Oct 11. Erratum in: J Virol. 2007 Mar;81(5):2538.
17 Gang Zhang, Dany Shoham, David Gilichinsky, Sergei Davydov, John D. Castello, and Scott O. Rogers. Correction: Evidence of influenza a virus RNA in Siberian lake ice. J Virol. 2007 March; 81(5): 2538. doi: 10.1128/JVI.02773-06 PMCID: PMC1865937
18 Worobey M.J. Phylogenetic evidence against evolutionary stasis and natural abiotic reservoirs of influenza A virus Virol. 2008 Apr;82(7):3769-74. doi: 10.1128/JVI.02207-07. Epub 2008 Jan 30.
19 Zimmer SM, Burke DS. Historical perspective–Emergence of influenza A (H1N1) viruses. N Engl J Med. 2009;361:279–285. [PubMed]
20 Nelson MI, Viboud C, Simonsen L, Bennett RT, Griesemer SB, St George K, Taylor J, Spiro DJ, Sengamalay NA, Ghedin E, Taubenberger JK, Holmes EC. Multiple reassortment events in the evolutionary history of H1N1 influenza A virus since 1918. PLoS Pathog. 2008 Feb 29;4(2):e1000012. doi: 10.1371/journal.ppat.1000012.
21 Wertheim JO. The re-emergence of H1N1 influenza virus in 1977: a cautionary tale for estimating divergence times using biologically unrealistic sampling dates. PLoS One. 2010 Jun 17;5(6):e11184. doi: 10.1371/journal.pone.0011184.
22 Oxford JS. Et al. Naturally occurring temperature-sensitive Influenza A viruses of the H1N1 and H3N2 subtypes. J Gen Virol (1980). 48, 383-389.
23 Scherer WF, et al. Vector incompetency: Its implication in the disappearance of epizootic Venezuelan equine encephalomyelitis virus form Middle America. J Med Etomol 23(1):23-29 1986 Jan 24.
24 Powers AM, et al. Repeated emergence of epidemic/epizootic Venezuelan equine encephalitis fro a single genotype of enzootic subtype ID virus. J Virol 71(9):6697-6705. Sept 1997.
25 Weaver, SC, et al. Genetic evidence for the origins of Venezuelan equine encephalitis virus subtype IAB outbreaks. Am J Trop Med Hyg 60(30): 441-448. 1999.
26 Braulty AC, et al. Potential sources of the 1995 Venezuelan equine encephalitis subtype IC epidemic. J Virol 75(13): 5823-5832 July 2001.
27 Rivas F, et al. Epidemic Venezuelan equine encephalitis in La Guajira, Colombia, 1995. J Infect Dis 1997;175:828-832.
28 Weaver SC, et al. Re-emergence of epidemic Venezuelan equine encephalomyelitis in South America. Lancet 1996 Aug 17 348(9025):346-340.
29 Scherer WF, et al. Vector incompetency: Its implication in the disappearance of epizootic Venezuelan equine encephalomyelitis virus from Middle America. J Med Etomol 23(1):23-29 1986 Jan 24.
30 Braulty AC, et al. Potential sources of the 1995 Venezuelan equine encephalitis subtype IC epidemic. J Virol 75(13): 5823-5832 July 2001.
31 Navarro J-C, et al. Postepizootic persistence of Venezuelan equine encephalitis virus, Venezuela. Emerg Infect Dis 11(12):1907-1915 Dec 2005.
32 Scherer WF, et al. Vector incompetency: Its implication in the disappearance of epizootic Venezuelan equine encephalomyelitis virus from Middle America. J Med Etomol 23(1):23-29 1986 Jan 24.
33 Abraham, T. Twenty-first Century Plague: The Story of SARS. Baltimore MD: Johns Hopkins Univ Press 2005. Is a short, useful summary of the SARS epidemic.
34 International Dimensions of Ethics Education in Science and Engineering: Case Study Series. IDEESE: Cases – Reporting Incidence of SARS: Appendix A. available at: http://www.umass.edu/sts/ethics/sars.html.
35 Zhuaang Shen, et al. Superspreading SARS events, Beijing, 2003 Emerg Infect Dis 2004 10(2):256-260. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3322930/#R1
36 MMWR. Update: Outbreak of Severe Acute Respiratory Syndrome – Worldwide, 2003. MMWR March 28, 2003 / 52(12);241-248. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5212a1.htm
37 WHO. World Health Report 2007 Ch 3: (illustration): Probable SARS transmission on flight CA112 in March 2003. http://www.who.int/whr/2007/media_centr ... g01_en.pdf
38 Singapore Ministry of Health. Biosafety and SARS Incident in Singapore September 2003. Websource: http://www.biosafety.be/CU/PDF/Report_S ... gapore.pdf
39 WHO Global Alert and Response: Severe Acute Respiratory Syndrome (SARS) in Taiwan, China. 17 Dec 2003. http://www.who.int/csr/don/2003_12_17/en/
40 Reuters: Taipei, Dec 20,2003. Taiwan says scientist likely got SARS in lab slip. Accessed at: http://www.royalsociety.org.nz/2003/12/ ... -taiwan-2/
41 Wu, W C et al. Development of Laboratory Biosafety Management: The Taiwan Experience. Applied Biosafety 12(1):18-25 2007. Accessed at: http://www.absa.org/abj/abj/071201wu.pdf
42 WHO. WHO post-outbreak biosafety guidelines for handling of SARS-CoV specimens and cultures. 18 Dec 2003. Accessible at: http://www.who.int/csr/sars/biosafety2003_12_18/en/
43 WHO Global Alert and Response (GAR). China reports additional SARS cases – update 23 April 2004. http://www.who.int/csr/don/2004_04_23/en/index.html
44 WHO Global Alert and Response (GAR). China confirms SARS in infection in another previously reported case; summary of cases to date – update 5. 30 April 2004. http://www.who.int/csr/don/2004_04_30/en/index.html
45 WHO Global Alert and Response (GAR). China’s latest SARS outbreak has been contained, but biosafety concerns remain – update 7. 18May2004. http://www.who.int/csr/don/2004_05_18a/en/index.html
46 Zhao Xiaojian, Zhu Xiaochao. China CDC Blamed for SARS escape. Caijing.com.cn Daily Update May 20, 2004. http://english.caijing.com.cn/2004-05-20/100013918.html
47 SCiDevNet website. Top Chinese Scientists ‘punished’ over SARS outbreak. July 8, 2004. http://www.scidev.net/global/health/new ... utbre.html
48 Zhang Feng (China Daily). Officials punished for SARS virus leak. Chinadaily.com.cn July 7, 2004. http://www.chinadaily.com.cn/english/do ... 344755.htm
49 CDC website. Remembering SARS: A deadly puzzle and the efforts to solve it. Online source: http://www.cdc.gov/about/history/sars/feature.htm
50 DEFRA. Declaration of a Protection Zone and Surveillance Zone 7Aug2007. http://webarchive.nationalarchives.gov. ... rz0807.pdf
51 HSE. Initial report on potential breaches of biosecurity at the Pirbright site 2007. Web source: http://webarchive.nationalarchives.gov. ... 0807b.htm/
52 Logan, P. Final report on potential breaches of biosecurity at the Pirbright site 2007. Health and Safety Executive September 2007. http://www.hse.gov.uk/news/2007/finalreport.pdf
53 Cottam EM, et al. Transmission pathways of Food-and-Mouth Disease Virus in the United Kingdom in 2007. PLosPathogens April 2008 4(4) e1000050. Web: http://www.plospathogens.org/article/in ... at.1000050
54 Juleff, N. The 2007 UK FMD outbreak: field investigation perspective. Institute for Animal Health (UK). PowerPoint presentation. Available online: http://www.fao.org/ag/againfo/commissio ... ctives.pdf
55 Klotz, LC and Sylvester, E. The unacceptable risks of a man-made pandemic. Bulletin of the Atomic Scientists. 7 August 2012. http://thebulletin.org/unacceptable-ris ... e-pandemic