by Ralph Nader
RalphNaderRadioHour
April 18, 2020
NOTICE: THIS WORK MAY BE PROTECTED BY COPYRIGHT
YOU ARE REQUIRED TO READ THE COPYRIGHT NOTICE AT THIS LINK BEFORE YOU READ THE FOLLOWING WORK, THAT IS AVAILABLE SOLELY FOR PRIVATE STUDY, SCHOLARSHIP OR RESEARCH PURSUANT TO 17 U.S.C. SECTION 107 AND 108. IN THE EVENT THAT THE LIBRARY DETERMINES THAT UNLAWFUL COPYING OF THIS WORK HAS OCCURRED, THE LIBRARY HAS THE RIGHT TO BLOCK THE I.P. ADDRESS AT WHICH THE UNLAWFUL COPYING APPEARED TO HAVE OCCURRED. THANK YOU FOR RESPECTING THE RIGHTS OF COPYRIGHT OWNERS.
Steve Skrovan: It's the Ralph Nader Radio Hour. Welcome to the Ralph Nader Radio Hour. My name is Steve Skrovan along with my cohost, David Feldman. Hello, David.
David Feldman: Hello. Good morning.
Steve Skrovan: And the man of the hour, Ralph Nader. Hello, Ralph.
Ralph Nader: Hey. How’s everybody in these troubled times?
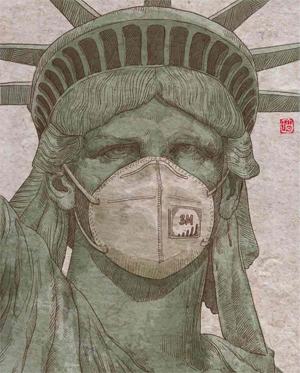
Steve Skrovan: Yeah. Well, we're all locked down. We're all locked down, but that doesn't prevent us from presenting the show. And we've got a great show for you. Of course, what's on everybody's mind is the coronavirus pandemic and this Covid-19 pandemic has laid bare many of the weaknesses of our healthcare system, including the health and safety of the healthcare workers themselves. The people we depend on who are at high risk during this crisis and despite the high risk, they are not being provided necessary protections. In fact, a headline in Fortune Magazine this week stated that some hospitals are telling healthcare workers they will be fired for reporting a lack of protective gear. Protective masks are usually used once and thrown away, but now faced with a very contagious virus, hospitals are telling doctors and nurses to clean and reuse their masks.
Some nurses report self-quarantining after being exposed to Covid-19 then being told to return to work before their two-week quarantine is up. Our first guest will be Jean Ross, who is President of the largest union of nurses in the United States, National Nurses United, and she is here to tell us about her efforts to help nurses stay safe during this pandemic. And that's just the first half of the show. And the second half, Donald Trump says he'd like to have the country reopen and back to normal by May 1st. When asked what he would rely on for that final answer, he pointed to his head, uh-oh, not a good sign. In the second half of the show, we welcome back Dr. Bandy Lee, who has been sounding the alarm about the mental health of this President and his judgment since she first appeared on our program back in 2017, to talk about the book she edited, The Dangerous Case of Donald Trump: 27 Health Professionals Assess a President. Last time Dr. Lee was here, just around the first of the year, she said, Donald Trump's thinks he's the "King of Everything."
And just this week at one of his press conference, he maintained that he had absolute power to reopen the country economically. Dr. Lee will tell us about why he is especially unfit to lead during this crisis, and as always, we'll find some time in between to take a short break and check in with our corporate crime reporter, Russell Mokhiber. And if we have some time left over, we'll try to tackle a listener question. Well, let's start by talking about what needs to happen to protect nurses. David?
David Feldman: Jean Ross is an acute care nurse and the President of National Nurses United. It's the largest union of registered nurses in the United States. National Nurses United aims to create a vision of collective action for nurses so that nurses are able to have more influence over the healthcare industry and a larger voice in public policy. Welcome to the Ralph Nader Radio Hour. Jean Ross.
Jean Ross: Thank you. I'm glad to be here.
Ralph Nader: Yes, indeed, welcome. I want to read one of the demands of the nurses just to illustrate how minimally they are in terms of the safety and health of workers in this area and also to show just how ill-prepared we were as a society. And I'm not just talking about the careening captain of the ship, the self-absorbed Donald Trump, who contradicts himself, overrules scientific advice and plays quack doctor. But we were unprepared because our public budgets are completely screwed up, going to massive redundant military budgets and at the expense of domestic necessities, which include saving lives, threatening injuries and preventing diseases. And that fell all over the institutions that weren't ready. Even CDC wasn't ready and fumbled.
So here's the demand and I'm quoting, "Employers shall provide the highest level of protection, including functioning negative pressure rooms and personal protective equipment for nurses providing care to possible and confirmed Covid-19 cases. Employers must ensure negative pressure rooms remain functional at all times during use. Highest level of personal protective equipment must include coveralls meeting ASTMs standards, gloves, temporary scrubs and other protections." Here we have hospital structures, many of them giant hospital chains with hugely overpaid CEOs—millions of dollars a year, some of them—as the California Nurses Association research pointed out years ago, and they weren't prepared. So what can be done here, Jean Ross, to take it from the workplace, the front lines all the way to Congress, all the way to the White House? Because the ultimate responsibility here for public health is the President of the United States and the Congress. They have the money; they have the power. They do have to work with the states and localities, but we have to go to the top if we're going to change the system and the priorities. Tell us about this.
Jean Ross: Well, it's going to take, obviously, a whole lot of pressure and we're hampered a bit now because of physical distancing. We're not out in the streets like we normally would be. So we've taken on a number of ways of changing this. In addition to our public petitions, the visual things we do. We have always lobbied Congress and starting today and in the next few days, we will be virtually meeting with senators from more than 20 states. We will be setting up appointments and asking for our two main asks, one of which you already mentioned, which is to urge Congress to mandate that the President use the Defense Production Act, not as he says as a hammer, but to actually use it to mass produce and get us needed PPE, ventilators and other medical equipment and get it now, as we would say, stat. And then also, to have OSHA do a temporary emergency infectious disease standard, and that would require that we get that optimal PPE [personal protective equipment] that you mentioned for all frontline healthcare workers.
So those are our two main asks. We've been on our nationalnursesunited.org site. We've had people take action; we have a website protectnurses.org. The public has been very helpful in doing that and we also have over 500 volunteers across the country to date. And we're texting every single nurse in the country. I don't think…well, I know we've never done anything like this before; I don't know that anyone else has. And we're offering a number of things--our online resources for information because, you know, we in the public are not getting the correct information; we cannot trust that. And then there are links to join our weekly Covid-19 Facebook live update. There is a Facebook group for nurses with all kinds of information about our advocacy efforts [including] the lobbying that I mentioned earlier. And so we're doing this peer-to-peer texting software. We've gotten many, many volunteers, over 500 and we reached over 750,000 nurses in 10 different states. Basically, if they are nurses, they can email us with a question at [email protected]. And there they can either use the information that we've got, email us, or they can, if they have a question, they can actually speak to someone on the phone from our union.
Ralph Nader: Well, even before the Covid-19 crisis, nurses have been much more visible than doctors. They've been out on the streets, informative picketing. They connect with citizen groups and they lobby for their patients on specific patient-oriented legislation. So I want to ask you, Jean Ross, what are your counterpart medical associations doing here? The American Medical Association, the Association of Family Physicians and all the others. What are they doing given the horrendous stories of unprotected healthcare workers [who] even when they get sick, don't get adequately tested, adequately served? What are the doctors of the country doing here?
Jean Ross: Well, what I've observed is they’re obviously as supportive as we are of getting the personal protective equipment because they're on the front lines with us. Although I don't see them necessarily getting coverage or being asked those questions as we are when I see them on TV. I will say, even for nurses, it depends on where you work. Not just what state, not even which state or hospital system, but actually what unit you work on. And that's just a result of course of our fragmented patchwork system where you can't tell any employer what to do. I mean even CDC guidelines are guidelines and those of course get downgraded every time the Hospital Association puts in a word. So we're just keeping at trying to inform the public because the public has always been solidly behind us.
Ralph Nader: You're right. Nurses are at the peak of public opinion support, but of course, doctors are on the front lines here. I was referring to the doctor organizations that have considerable influence over Congress and over the political system--from Washington to state capitals. What do you think they should be doing that they're not doing? These are the doctor specialty associations, the American Medical Association [AMA], its state chapters. What do you think they should be doing along with what you're doing?
Jean Ross: Well, I think they should be supporting us. I think they should be doing exactly what we're doing. Especially since very often, you know, we're a female-dominated profession and sad to say, sometimes they listen to men and the bulk of doctors still are more male. But you know when it comes to the kind of fighting that we do with our union, an organization and association is a lot different than a union and there aren't very many doctors that are unionized. So whereas we can speak out freely without fear of losing our jobs even during a pandemic, nurses are being threatened with being fired, they're not in the same position that we are. But absolutely I would hope that they would be lobbying for the same type of things for themselves and for us, and of course, for the public health.
Ralph Nader: Well, there's such heartbreaking stories where when patients get diagnosed with Covid-19, they have to be quarantined. They have to be isolated, sometimes from their own family. Oftentimes, if they're in nursing homes, families can only look through a glass window to try to communicate with them. What are the nurses doing about the kind of isolation, which of course leads to tremendous psychological damage along with the tremendous pain that these people are going through? And the nurses know what the situation is. What are they proposing here?
Jean Ross: Well, you know, we do our best obviously whatever situation we're put in. When those patients are in that situation where they can't have family with them, especially when they’re going to die, the nurse becomes that family. We are the ones that sit there and hold hands and tell them, you know, we're going to be there for them no matter what. There isn't too much you can do about that isolation because of where we're at right now with the virus. I mean, it has to be that way. That's understood. One of the things I wish fervently that we could get the President and the government to do is to ramp up testing and at least test healthcare workers first. That would let us know that for one thing, we're not spreading it from patient to patient and to the public when we leave the facilities every day, that kind of thing. But, I don't know that people recognize or would think of right away [is] how hard it is for nurses and other healthcare workers to see that amount of deaths every day, every shift. It is more than heartbreaking.
Ralph Nader: On that point you just made, you know, we have Governor Cuomo [and] President Trump start s speculating about reopening new economy and ending the lockdown. Well, just in the last few days, the death toll in New York state alone was over 700 a day. That's on the average, one death every two minutes, for the 24-hour period. It’s staggering. So what are the nurses preparing here when the politicians start heeding the business community and saying, well, this is the price we're going to have to pay; we can't lock down the economy for a long time; open up. What are the nurses preparing to do and say?
Jean Ross: Well, we're already, you know, I mentioned our actions, we do visual things [like] standing up outside of hospital facilities six feet apart, forming our own line, continuing to inform the public and hoping that they, with us, will insist to listen to the right information from medical experts and not economic advisors. I mean, this is just—there's going to be an awful lot of PTSD [post-traumatic stress disorder] now and when this is over. It will be the essential workers, not just healthcare workers; it will be the patients' families. It's very hard in our country. I mean, we all know that we don't really have a healthcare system. There's nobody been really concerned with it other than maybe the nurses, which is why we have pushed for Medicare for All for so long. This kind of illuminates exactly why we have needed something like that, and the public, even before the pandemic, was starting to understand that.
Ralph Nader: Let me suggest a different venue for your demonstrations. If you could demonstrate six feet apart in front of the White House with the proper signs and the nurses in white, it would have a much greater effect nationally through the media. And it's all free speech as long as you stay six feet apart; 20/30 nurses can do this, and do it again and again. There is nothing in front of the White House. In fact, no matter how terrible this president has been on many other issues, he probably has been picketed less than other prior presidents. It's as if he's too terrible to deal with. So I would suggest that. Now do you think after this Covid-19 relents that there's going to be a decisive push in public opinion and other healthcare worker organizations for full Medicare for All [with] free choice of doctor, nurse, hospital, whatever--much more efficient, much more lifesaving? Do you think it's going to change the equation here or it's just back to business as usual?
Jean Ross: I think the tendency in this country is always to go back to business as usual. It's easier and it's safer for whatever reason, but we won't stop pushing. And as I said, this is a great example. It shows people exactly why, for example, you cannot rely on being employed for your insurance. Everybody's not working now; a large percentage of us aren't. So [change] is going to continue to take pressure. But yes, I do see signs of that changing. We saw it even before the pandemic.
Ralph Nader: Do you think that the example from Canada will start having more of an impact? I've always been amazed. I wrote an article, ‘25 Ways Life is Better in Canada’, because they have a full Medicare for All system. It’s much more efficient. It comes in at half [the] price per capita and they cover everyone. [Here] 30 million people are uncovered, another 50 [million] under- insured. Anywhere, according to a Yale study that just came out recently, [between] 65,000 to 105,000 people die every year because they can't afford health insurance to get diagnosed and treated in time on and on. Tell me, you're connected with the nurses in Canada. Why hasn't this country paid attention to it works in Canada? It's not theory; it's not some wild projection. It's been working since the late 1960s.
Jean Ross: Right. Well, of course we do use them as one of the examples. We had several examples including Canada. People do, they are starting to listen to that. They want a lot of what they've got. People who are dead set against anything like universal health, Medicare for All, will use anecdotes and old wives’ tales about people dying there because they can't get surgery and that kind of thing. But I think what's telling is for people in any country that have what Canada has, that when that health system is threatened to be taken away or changed, like some of our multinational corporations are trying to do, they would just assume that all those countries with health plans like that have what we have that people rise up and say No. We haven't gotten to a point where we're close to having it. The closest we've got is Medicare. When Medicare gets threatened, people here step up and say, "Don't you dare." We have to get them to the point, which we may be at that point now, where they say, "We need this too."
Ralph Nader: Well, one difference between Canada and the US was in the 1960s, we were embroiled in the Vietnam War and they weren't and the reason why Lyndon Johnson didn't get Medicare for All in the 1963-64 period when Medicare and Medicaid were enacted, was the that Congress said to them, there is too much deficit; the Vietnam War is costing us too much. You just have to do it for the elderly and under certain conditions for the poor. So once again, the military machine devours its own people and we're still inheriting that terrible missed priority that Canada didn't have to endure. What do you see in the next 6, 8, 10 weeks, Jean Ross?
Jean Ross: Well, we of course are going to continue to do our push. We will raise holy hell if he decides economically to open the country and to do it as stupidly as he did the beginning of this where he didn't take control. I think you're going to see unfortunately, unless and until we get the PPE that we need and want, we are going to see more and more healthcare workers struck down. And that will put the system that we have more at risk than it is now. Because it isn't just a statement, I think we can all see what will happen as we continue to get sick. You cannot afford to have us not working.
Ralph Nader: Well, you get feedback from nurses all over the country. And I'm curious about why haven't the Southern states that have their own big cities, [such as] Houston, Phoenix, Atlanta, Miami, come down with levels of severity that have affected New York, New Jersey, Detroit, some parts of Illinois? I know New Orleans has come down with it severely. But what's going on? Do you think that they had a heads-up and they locked down because it started in hotspots like New York and New Rochelle?
Jean Ross: You know, I'm not sure what he does with his friends versus the rest of us, but I will tell you that, you know, they keep talking about waves of the disease; Dr. Fauci keeps talking about that, so does Governor Cuomo. There will be and they just might not be at that point. Florida nurses are very worried. They're extremely worried. I myself live in Minnesota. We, I think, locked down early enough that we are being able to handle what we've got here. But we're preparing for more. We're not planning on opening up soon. So it depends on where you are in the illness. But people that are very cavalier, that think because they're in a rural community, for example, they could be horribly hard yet. They are the places these for-profit employers have closed hospitals. There will be fewer places for those patients to go and their system will be overwhelmed very readily.
Ralph Nader: Well, Scott Gottlieb, who was the former Food and Drug Administrator, chief for Trump--he's very close to the drug industry and he's now out of government--just gave an interview saying that there's not going to be a vaccine for two years. And whether there will be anything intermediate, by way of lessening the severity of the Covid-19 affliction, is still unknown. And there is a lot of quackery going on. You have the President of United States recommending a dual drug that can damage the heart, has bad side effects, and there's no evidence that it [positively] affects Covid-19 patients. And then on the internet [are] crazy schemes and nostrums and wild assurances--a corporate crime wave. And the government is just not putting enough prosecutors on to make examples of these criminals. So we have such breakdowns coming. All the latent insecurities of our political economy and the plutocratic control of it--of the many by the few--are coming to the forefront here. And if there's a second wave in the fall and it affects the election, we have even more chaos. Who gives us reassurances here? Who can say that the supplies are now going to be adequate, that the hospital facilities are now going to be adequate? Can the military play a major role here? They warned Trump in September with a hundred-page report; it was just revealed that it predicted almost exactly what happened with the Covid-19. And it was ignored by the White House. So where do you see the leadership, the reassurance?
Jean Ross: Well, it's not real hopeful. I mean, you know. Okay. You mentioned Trump, not only is he not doing enough, he's actually sabotaging what should be done. That's our lobbying for the DPA, the Defense Production Act being invoked. As far as the equipment that we need, they keep talking about a shortage. We're not sure how short they are. They are doing battlefields triage, making nurses wear the wrong equipment or bring bandanas to work and they say, this is in order to save. Well, when an employer tells us to save, it's all economical. I know they want the public to think they're just trying to conserve supplies so there'll be enough for how long this thing lasts, but it's not. It's money! We know that, because we see the equipment at some of the hospitals under lock and key and they tell you, you can't have it. The hand really doesn't know what the foot is doing. It's got to be Congress. I know the House is trying. They tried to get that temporary OSHA standard in one of the relief packages; they haven't been able to do it so far. But until you get someone to control that man and make him do what is needed for the health of the public, things aren't going to change.
Ralph Nader: Well, we're talking with Jean Ross, the President of National Nurses United. You know, I've accused Congress of being AWOL. You know that almost a month ago, they just went back home--no hearings, no committee meetings, no floor debate. And I said, well, they must not think they're essential service, that they're not essential workers, because within a few hundred yards of the Congress are all kinds of people on the front lines exposing themselves to peril and doing their duty and work. I think there needs to be high-profile congressional hearings. Have you put your laser beam pressure, Nurses United, on both the House and the Senate on this? They are coming back on April 20; who knows for how long. I've never seen a situation like this. They're not on the job.
Jean Ross: No, they're not. You know, even our nurses have asked what we can do about Trump and quite frankly, you know, the man is ill. We know that. I honestly don't hold any hope of him doing what he needs to do, other than maybe seeing him removed. But it's got to be the people who are enabling him who know better, the ones that aren't ill. They should be doing that. They should be doing their duty. And I am hoping, and certainly, we would support investigations into exactly what's going on. We're looking right now at where the heck our equipment is.
Ralph Nader: Well, I think the spotlight has got to be on Congress, but also of course, greatly on Trump who is using these daily news conferences to try to enhance his re-election and to take credit for everything and responsibility for nothing. He gives himself a 10 on a scale of 10, saying he has no responsibility for anything that's gone wrong. So in addition to the six-feet-apart demonstration in front of the White House, why don't you invite President Trump in full hazmat equipment to one of your hospitals to see exactly what you've been facing? Why don't you invite him? I mean, he's a draft dodger to be sure, but you know, he likes to be in the spotlight. [Jean chuckles] This will get them on the news like nothing else.
Jean Ross: Well, it certainly would make a good visual. I actually did hear one of the doctors on TV suggests that from New York last night. He needs to come down here when he spouts off and says "everything's under control; we're doing a great job." He needs to be on one of those units.
Ralph Nader: How do people reach National Nurses United? Can you give their website?
Jean Ross: Yeah. If I were the public, and were looking for information and help, I would go to nationalnursesunited.org or protectnurses.org. If I were a nurse, I would go to [email protected].
Ralph Nader: Well, thank you very much, Jean Ross. We’re entitled to be very proud of the millions of nurses all over the country who do work almost nobody would dare to do and don't get much publicity for it. I think if the nurses want to get more attention, they should learn how to put a ball in a hole in the ground, like golfers and win The Masters and then they’ll get attention all over the world.
Jean Ross: There you go. Well, thank you for helping us get the word out.
Ralph Nader: You're very welcome.
Steve Skrovan: We have been speaking with Jean Ross, President of National Nurses United. We will link to their work at ralphnaderradiohour.com. Now we're going to take a short break. When we return, we will talk to Dr. Bandy Lee, a forensic psychiatrist at Yale, who thinks the pathology of Donald Trump is a real threat to the public health. But first, let's check in with our corporate crime reporter, Russell Mokhiber.
Russell Mokhiber: From the National Press building in Washington, D.C., this is your Corporate Crime Report on Morning Minute for Friday, April 17, 2020. I'm Russell Mokhiber. In the years since the 2008 financial crisis, federal prosecutors in the United States have brought dozens of criminal cases against the world's most powerful banks, charging them with manipulating financial indices, helping their customers evade taxes, evading sanctions, and laundering money. To settle these cases, global banks like UBS, Barclays, HSBC, and BNP Paribas paid tens of billions of dollars in fines. They also agreed to extensive reforms, hiring hundreds of compliance officers, spending billions on new systems, and installing independent monitors. In effect, the banks agreed to become worldwide enforcers of US law, including financial sanctions. That's a take of University of Virginia law professor, Pierre [-Hugues] Verdier, author of the just released book, Global Banks on Trial: U.S. Prosecutions and the Remaking of International Finance. For the Corporate Crime Reporter, I'm Russell Mokhiber.
Steve Skrovan: Thank you, Russell. Welcome back to the Ralph Nader Radio Hour. I'm Steve Skrovan along with David Feldman and Ralph. In response to state governors pushing back on his claim of absolute authority over when to reopen the country, Donald Trump tweeted out a reference the film Mutiny on the Bounty, effectively comparing himself to the infamous captain Bligh, the volatile and paranoid captain of the bounty. He's calling himself this. For the last three years, our next guest has been arguing that the mental health of our President mandates that he too should be set afloat in a dinghy. David?
David Feldman: Dr. Bandy Lee is a forensic psychiatrist at Yale School of Medicine and an internationally recognized expert on violence. Dr. Lee is the President of the World Mental Health Coalition and has worked with various governments to implement violence prevention programs in prisons and the community. Dr. Lee edited the book, The Dangerous Case of Donald Trump: 27 Psychiatrists and Mental Health Experts Assess a President. Welcome back to the Ralph Nader Radio Hour, Dr. Bandy Lee.
Dr. Bandy Lee: Thank you very much for having me back.
Ralph Nader: Well, you've made your point again and again with your colleagues from all over the country and the world that President Trump is unfit for his responsibilities of office. Not just politically disagreeable, but that he has levels of instability, levels of confusion, unable to process information to make rational decisions, completely absorbed with his own ego through which he interprets everything--scapegoating, attacking people who dare to criticize him and using massive torrents of flattery for the people who are his sycophants. It's hard, you know, to visualize the captain of a ship careening wildly in turbulent waters, called Covid-19, having delayed for weeks by ridiculing this peril in a variety of ways, which he now denies, and increased certainly the level of deaths and afflictions as a result, before any measures start being put in order. Now, there is a convention in your profession that you don't make a judgment about someone's mental health unless you're sitting there examining the person. And you have raised this issue with your profession, and you have responded to it. Tell us.
Dr. Bandy Lee: Yes, that's right. Well, I think it has shown itself to be critical. The fact is not so much, the important fact is not that that convention prohibits diagnosing public figures. Actually we would have no need to. They're not our patients. We wouldn't examine them. So there's nothing left to be confidential about, but what was truly alarming to me, and I think egregious on the part of the American Psychiatric Association, for whatever reason they did it, at the onset of the Trump presidency, changed the rule to cover not just diagnosis, but any comment of any kind on a public figure under any circumstance. Now that blatantly goes against our First Amendment rights because a public figure is not a patient; it's not covered by professional responsibility. Our professional responsibility is to society. In fact, that very rule, which is only one rule in one voluntary association; none of the other associations around the world that we know of has this rule and no licensing board can adopt it because it goes against the First Amendment.
But the fact that they prevented our ability to warn society in the case of dangers, stating this rule, when it's not in fact even a rule, it's a guideline; the guideline actually states this. We don't just have a responsibility to patients. We have it as well to society. And so psychiatrists are expected to participate in activities that improve the community and promote public health. That is why that restriction is in there. So, in the context of the public asking us about a public figure, we're encouraged to educate the public, just not diagnose. And by amplifying the diagnosis and eliminating the fact that we ought to educate the public or protect public health is really turning medical ethics upside down and that is what happened at the onset of the presidency. And I think that needs to be clarified that on an association, that not even all psychiatrists belong to, has been engaging in this misinformation campaign, because it was really a public campaign and intimidation of mental health experts when they would wish to speak.
Ralph Nader: How about the American Psychological Association? Where did they stand on this?
Dr. Bandy Lee: That's very interesting because when the American Psychiatric Association came out with this announcement of what they call the "reaffirmed rule," but it's actually a new rule, the American Psychological Association said, we have a similar rule ourselves. Of course they don't, and they would later retract that statement, but that's what happened.
Ralph Nader: Well, you have the 25th Amendment; it’s the Constitution, which really sets the stage for your kind of professional judgment and the 25th Amendment says if the Vice President of the United States notices erratic behavior, unstable behavior, whether psychological or physical disability, the Vice President can put in a motion with other cabinet members, an initiative to suspend the President from his or her office. Now, if they were to do that, they would have to resort to the kind of empirical evidence and professional judgment that you're putting forward. Would they not?
Dr. Bandy Lee: Exactly. Exactly. In fact, I have had a number of conversations with the drafter of the 25th Amendment, because we've been invited to a number of conferences to speak together. And he has lamented the fact that the 25th Amendment, because it is a political process and because it is political, "I don't have a role in deciding whether or not the 25th Amendment happens, but it could not happen and would not be sensitive enough to happen in many psychiatric circumstances where it ought to be initiated by the input of mental health experts such as myself. And that is something that I find truly problematic and even exceptional in all legal cases." As a forensic psychiatrist, I'm often called to testify as an expert witness and in courts in numerous legal cases, in policy decisions, they would not make a decision without expert input. I mean the fact that you admit evidence into court, an expert opinion is considered when it's done in the standardized way was scientific backing of it. It is considered evidence. In fact, it's part of the facts that you gather. And therefore for political process to say, or for political people to say that a political process should not engage with anybody else other than politicians is quite a divergence from usual legal practice.
Ralph Nader: They couldn't engage it without evidence. They'd have to produce evidence of the kind that you are bringing together.
Dr. Bandy Lee: Exactly.
Ralph Nader: You know, it's quite interesting. A president should tell the truth to the people. A president that has 17,000 fabrications and lies since he was inaugurated. He is a pathological liar. He is a savage sexual predator. He misleads his supporters and endangers them. He urges them to do things that are not good for them, like taking certain unproven drugs for the Covid-19 and he contradicts scientists with his political attempt to embellish his own ego and his own achievements in preparation for the next election. Now to me, an impeachable offense is sufficient with a pathological liar. How can you have a president that every day, sometimes every hour, tweets out fabrications, things that aren't so, things that didn't happen, things that he thought happened that didn't happen, things that he did that he didn't do in terms of taking credit. So it's really a very easy case on many, many grounds. And are you getting any support from other professions like medical societies, nurses’ organizations who have to deal with similar phenomena and have similar professional duties, not just to individuate themselves with personal clients, but their professional commitment to the society at large? That's one of the definitions of a profession.
Dr. Bandy Lee: Yes. In fact, now that he is increasing the unnecessary deaths from the viral pandemic, not just in the hundreds of thousands, but possibly in the millions around the world as he pulls funding from the World Health Organization. I mean the one instrument we have for bringing about global coordination for confronting this crisis, there couldn't be a greater medical immediate emergency as we have now, all because of the psychological problems of this President as well as his criminal intent. But we have the situation here and so there's no question among medical professionals. There's a group of non-psychiatric physicians who are now backing us and collecting their voices. Of course, among mental health professionals it has always been a consensus apart from just a handful of outliers. And yet, our media in this country, talk about the deadliness from denying expertise that the media has engaged in starting with the New York Times editorial board actually collaborated with the American Psychiatric Association in January of 2018 to put out a very explicit statement that the public does not need to hear from psychiatrists about the President's mental health, that they should not speak and that their opinion is not wanted. I mean, what kind of newspaper does that? But of course that was the explicit voice of not just the American Psychiatric Association, but a very pharmaceutical industry supported past APA president, who was the only full-page opinion that the Times has ever printed on this issue, who said the president is just a jerk. And so to this day, the members of the public come to us and say, why aren't mental health professionals speaking up more? And why, when the only psychiatrist they hear of is someone who says that the President is just a jerk when even for them, it is so blatant that the President is suffering from severe symptoms? And as you say, the level of lying alone, is pathological.
Ralph Nader: We're talking with Dr. Bandy Lee of Yale School of Medicine. The New York Times, Bandy, has published hundreds of articles about the incompetence of Trump, the ignorance of Trump, the incapacity to govern of Trump, the petty, vengeful nature of Trump, the nepotism of Trump, the chronic lying of Trump. So if they don't want to use your language, your psychiatric or psychological language, what is it about them that they don't go to the conclusion of their own reporters’ documentation and say he's unfit for office? He's totally incompetent and he creates a fantasy about himself and separates people who believe him from reality in their daily lives and he should resign. He should obviously have been impeached if the House of Representatives took proposals from constitutional law specialists, he could have been impeached on 12 grounds. But apart from that, there should be a mass demand for his removal, for his resignation.
Oh, he'll never resign. Well, that's not the burden of those who demand his resignation. That's their duty. And they used to say Nixon would never resign--he's stubborn; you have to take him out feet first. Well, he did resign, and it's appalling to see this marvelous documentation by newspapers and other media day by day of the wreckage that he is leaving the country embroiled in, and aiding and abetting actually worsening trends. Like he wanted to cut the budgets of key health agencies in the country that dealt with infectious disease and he closed down the office in the White House headed by a rear admiral to prepare for a potential pandemic in 2018. It's not that he’s just doing nothing in moments of peril and not just Covid-19; he's actively aiding and abetting devastations to health and safety of the American people, whether it's cutting back OSHA, whether it's destroying EPA, whether it's freezing the activity of the auto-safety agency [NHTSA], whether it's wanting to get rid of Obamacare without any replacement and expose 20 more million people to life without health insurance, which includes a consequence of mortality and morbidity as a result.
So what's the New York Times’ problem here? If they don't want to use your language, they have ample evidence in their pages.
Dr. Bandy Lee: Well, you have just outlined a great summary of the multiple ways in which he has been destructive to the country and if not to the world. And this destructiveness, if it were purely criminal, purely intentional, that is, then it would go only so far. But the reason why it is critical to distinguish what is pathological versus normal and healthy and ordinarily life affirming is that it actually ends up being far more efficient. And people marvel at the fact that he's such a "Teflon President" or that he is able to whip up a following in ways that no one ever has managed to. Well, this is actually a symptom of pathology. And the reason why it's so important to distinguish is exactly for the factors you outlined, that he ends up being almost exclusively destructive and never productive. Because pathology is so efficient, it brings about damage and death and it is far more effective than anything we can consciously, rationally plan. And that's also what's happening in addition to the criminal intent. And so why the New York Times avoiding our language? I mean it set the stage. The media were not always like this. In fact, I was interviewing 15 hours a day, every single day, soon after the publication of our book, The Dangerous Case of Donald Trump, which was an unprecedented, near instant New York Times bestseller. Well, they avoided reviewing it. They avoided mentioning it and eventually when our voices were getting so loud that our topic became the number one issue of the national news. All the programs were airing us; all of the major network, cable and primetime programs had or were mentioning us on air. That is when the New York Times stepped in. Why did they do so? I couldn't really speak for their intentions, but I could speak the results of their actions.
Ralph Nader: Did they ever explain? Did they ever have an intelligent exchange of views to explain your position?
Dr. Bandy Lee: No, no. I mean, even the reporters who quoted me as central to their articles had only my quotes taken out; all the political pundits would be left in, and they themselves have been puzzled. It's happened over and over, not just with the New York Times now, but with multiple, certainly the most prominent media. And I had been invited to news programs and other major programs, over 50 times just for CNN. And none of them were, none of them were actually aired except for one. They would all get canceled at the top. So producers would constantly be inviting us, and editors and reporters would constantly be interviewing us. But it would never get printed. And after two and a half years, almost two and a half years of this, we finally realized it's not by chance. And my guess is that if you exclude expert voices who can show you the standardized means by which we come to our conclusions--they're not just personal opinions--there are professionally standardized conclusions that we come to consensus about once we have enough information. And most experts will tell you we have more information about Donald Trump than any patient that we've ever treated. It was even laughed about at a major conference at Harvard. And so when we have this much information and this much confirmation and the President has not met one criterion of basic mental capacity, that is the fundamental building block of fitness. And so if you don't have that, if you don't have rationality and sanity, you can't have any other kind of fitness. And he did not meet one criterion, and we had great information for that report, which came from the Mueller report.
Ralph Nader: Let me propose to you a question probably you've never been asked, about the bizarre nature of what it takes to demand a president to resign. So let's say hypothetically, Donald Trump had a national news conference tomorrow and he said, ‘to my tens of millions of supporters, you've supported me because I say publicly what you think privately, and I am going to say the following.’ And he launches into the most ugly, bigoted stereotypes, against Hispanics, against Blacks, against Asian-Americans, against Jews, against Arabs, against gays. And then he said, ‘Take that’, my guess is the New York Times would immediately demand his resignation, because words are more explosive than devastating deeds in American politics. What's your view?
Dr. Bandy Lee: First of all, I'm not sure the New York Times will make a demand even in that state, partly because I had been hearing about the conflicts of interests that some reporters have and [interrupted]
Ralph Nader: Well, let’s not get mired in that right now. The media would demand his resignation. The public would demand his resignation. You see it all the time. Terrible politicians, terrible record for four or five years, stiffing workers, stiffing consumers. They may stumble on some bigoted words and they’re told to get out.
Dr. Bandy Lee: Oh, I see. Well, because as you said, the President is speaking other people's minds, and wouldn't that in sure political terms be something that is acceptable. So I guess my argument still is going in the direction of they're not demanding his resignation, but what would allow for the kind of turnaround among his base or his followers, that would allow for a demand for resignation to be possible, is actually psychological--not based on words or objective words or deeds. And that is if the President were to say, ‘I made a mistake; this warrants resignation’. Then that is a point where a large portion of his followers will turn around and agree with him--not the widespread deaths from Covid-19 and not the loss of family members and friends--but the President either saying so himself or being forced to resign. The resignation itself or the impeachment itself, I have said over and over, justifies impeachment in the minds of his followers. And that is because their psychology is at a level oftentimes--I should note that people are drawn to the President because of similar psychology to start with; others are healthy and sound to begin with. But because of the length of time that a severely symptomatic President has been kept in power and the position of influence with lots of exposures through the media and social media and rallies, there's also been a transmission of symptoms; mental symptoms can be transmitted. And so you end up with a base that is very much psychologically similar to the President. And this psychology, unlike most people's impression, is actually submissive psychology. And Donald Trump, he has to maintain a posturing of being dominant and powerful and strong. But we have seen in multiple situations under the influence of Vladimir Putin or Kim Jong-un, he quickly comes to state of submissiveness. And that means that once someone is removed from a position of power or he admits to a mistake, in other words, shows that he is fallible, then the unconditional worshiping of that person ceases. And it's actually a very binary, simplistic dynamic where they either idealize him as perfect, like a king, like a God with total authority over all situations, or he is too weak, too fallible, too human to be worth following.
Ralph Nader: Well, you know, he's never admitted a mistake. He's never admitted doing anything wrong. His phrase is, ‘I have not done anything wrong’. He said under Article II, ‘I can do anything I want as President.’ Those were his very words. So what you're really arguing was anticipated by our founding fathers. Number one, the last thing they wanted to tolerate was a monarchical executive, another King George, that violated accountability, which is why they set up the separation of powers between the legislative executive and judicial branches. And what you're arguing falls right into a major category of what they thought was an impeachable offense in the Federalist Papers, which was "an abuse of public trust". That was written by Alexander Hamilton, among others, who believed in a strong president. So it's not like, you know, you're on the margins of professional expression here. You can document it in a whole variety of secular ways-- historical, contemporary, functional, you name it. Well, we're out of time. Thank you very much, Dr. Lee. It’s to be continued.
Dr. Bandy Lee: I hope so. Thank you very much.
Steve Skrovan: We've been speaking with Dr. Bandy Lee about Donald Trump's mishandling of the coronavirus crisis and other things. We will link to her work ralphnaderradiohour.com. So we have time. Let's do a listener question. David?
David Feldman: This one comes to us from Paul D. Marshall. "Ralph, on a lighter side, how do I purchase the Nader family cookbooks, The Ralph Nader and Family Cookbook: Classic Recipes from Lebanon and Beyond and [It Happened] In the Kitchen: Recipes for Food and Thought. [https://www.thriftbooks.com/w/it-happened-in-the-kitchen-recipes-for-food-and-thought_nathra-nader_rose-b-nader/422343/#isbn=0936758295&idiq=1752850] Thank you. Great show. I'm a regular listener. Hope you all stay well.
Ralph Nader: Thank you, Paul. Well, it's a great cookbook and I don't say that for myself. They're mostly my mother's recipes and we grew up on them--very nutritious, delicious, low in fat, sugar, salt. But it's more than a cookbook. I read a long introduction of what food around the table meant in terms of raising us and having conversations and training us not to whine about the food and to understand nutrition and not to be susceptible to sweetened food and additives. You can get the book from any bookstore, but the bookstores are closed so you'll have to get it online. You know where you can get books online—Powell’s is one, Barnes & Nobles, and other, the dreaded Amazon is a third. And if you want to have bulk copies, you can go to the publisher. It's a beautiful hardback book with all kinds of beautiful photography of the various dishes and the publisher is Akashic Books. That's A-K-A-S-H-I-C Books. You can reach them at acashicbooks.com. Thank you very much, Paul.
David Feldman: You know more and more, people, because they're quarantining, sheltering in place, are cooking, and I can't tell you the number of people who have discovered their kitchen and are eating healthy.
Ralph Nader: And in a sense by encouraging more nutritious diets and less fat, sugar, salt, diets, junk-food diets, you're improving your resistance to any kind of affliction. Healthier people have a better chance.
Steve Skrovan: Ralph, your mom taught you a lot of things. Did she teach you to cook?
Ralph Nader: Yeah, we had to help around the kitchen. There were certain things like elaborate desserts that she learned years ago and required very adept handling that we weren't involved in doing, but you know, making hummus, different kinds of soups, appetizers, salads, borehole (sp?) with garlic and onions, lentil soup, all kinds of legumes. Yeah.
Steve Skrovan: Would you consider yourself a decent cook?
David Feldman: He was a cook in the army! Weren’t you a cook in the army?
Steve Skrovan: I said decent cook. [lots of laughter]
Ralph Nader: Yeah. That’s really cooking for volume, David. I once was involved in an effort of making banana bread for 24,000 soldiers.
David Feldman: Wow. That's a lot of bananas.
Ralph Nader: This is simple cooking. That's the great thing. These recipes are simple to follow. You can use your own judgment and vary it, and they involve ingredients that are available, with few exceptions, in all the grocery stores, and they're less expensive than heavy cuts of meat and pork.
Steve Skrovan: All right, very good. Thank you for your questions. Keep them coming on the Ralph Nader Radio Hour website. I want to thank our guests again, Nurse Jean Ross and Dr. Bandy Lee. For those of you listening on the radio, that's our show. For you podcasts listeners, stay tuned for some bonus material we call "The Wrap Up". A transcript of this show will appear on the Ralph Nader Radio Hour website soon after the episode is posted.
David Feldman: Subscribe to us on our Ralph Nader Radio Hour YouTube channel, and for Ralph's weekly column, it's free; go to nader.org. For more from Russell Mokhiber, go to corporatecrimereporter.com.
Steve Skrovan: And Ralph has got three books out, 1) the fable, How the Rats Re-Formed the Congress. To acquire a copy of that, go to ratsreformcongress.org. 2) Fake President: Decoding Trump’s Gaslighting, Corruption and General Bullsh*t, co-written with Mark Green, and 3) The Ralph Nader and Family Cookbook: Classic Recipes from Lebanon and Beyond. We will link to that also.
David Feldman: The producers or the Ralph Nader Radio Hour are Jimmy Lee Wirt and Matthew Marran. Our executive producer is Alan Minsky.
Steve Skrovan: Our theme music, "Stand Up, Rise Up", was written and performed by Kemp Harris. Our proofreader is Elisabeth Solomon; our intern is Michaela Squier.
David Feldman: Join us next week on the Ralph Nader Radio Hour when we welcome back, one of the foremost experts in infectious disease, Dr. Michael Osterholm. Thank you, Ralph.
Ralph Nader: Thank you everybody. And it's more important than ever for citizens to be all over Congress. We're going to try to have a resurgence here, learn from the defenseless posture of our country in the Covid-19 and get some real changes and it's all about Congress. And that's why I wrote this book. Just go to ratsreformcongress.org.