by National Nurses United
Accessed: 4/25/20
https://www.nationalnursesunited.org/covid-19
NOTICE: THIS WORK MAY BE PROTECTED BY COPYRIGHT
YOU ARE REQUIRED TO READ THE COPYRIGHT NOTICE AT THIS LINK BEFORE YOU READ THE FOLLOWING WORK, THAT IS AVAILABLE SOLELY FOR PRIVATE STUDY, SCHOLARSHIP OR RESEARCH PURSUANT TO 17 U.S.C. SECTION 107 AND 108. IN THE EVENT THAT THE LIBRARY DETERMINES THAT UNLAWFUL COPYING OF THIS WORK HAS OCCURRED, THE LIBRARY HAS THE RIGHT TO BLOCK THE I.P. ADDRESS AT WHICH THE UNLAWFUL COPYING APPEARED TO HAVE OCCURRED. THANK YOU FOR RESPECTING THE RIGHTS OF COPYRIGHT OWNERS.
About the Novel Coronavirus (COVID-19) Outbreak
In December 2019, a newly identified coronavirus, known as COVID-19, emerged in Wuhan, Hubei Province, China causing illness in humans. Multiple clusters of COVID-19 have since been reported across China and in more than 70 other countries including Italy, Iran, Japan, South Korea, and the United States.
The U.S. Department of Health and Human Services declared the virus to be a nationwide health emergency following the World Health Organization’s (WHO) declaration of a public health emergency of international concern on January 30, 2020.
On January 21, 2020, China announced for the first time that health care workers have been infected- at least fourteen by recent counts. In recent days, dozens of U.S. health care workers have been exposed due to their employer’s lack of protections.
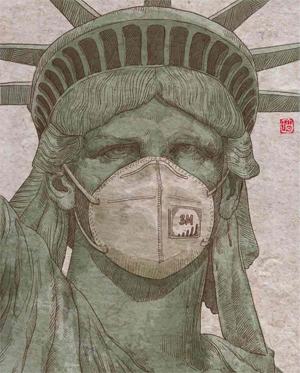
Health care workers need your help in the fight against COVID-19.
Click below to call for safer facilities, more PPE, and thank nurses for all that they do.
TAKE ACTION
About COVID-19
While much has been learned about COVID-19 in a few weeks, there is still a lot we don’t know:
About the Virus
What is known: It is a coronavirus, which is a large family of viruses that can infect animals and/or humans. COVID-19 is similar to the viruses that cause SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome).
Symptoms
What is known: Several published reports have established a basic picture of clinical symptoms and outcomes for those infected with COVID-19. These symptoms can include fever, cough, muscle soreness, weakness, diarrhea, headache, and other symptoms. While some symptoms appear to be common, there is also diversity in how COVID-19 manifests (Table 1).
Table 1: Symptoms of COVID-19 Reported in the Scientific Literature
Symptom / Huang et al. (Feb 15-21, 2020), report on 41 admitted hospital patients with laboratory-confirmed COVID-19 infection in Wuhan, Hubei Province, China[1] / Wang et al. (Feb 20, 2020), report on 105 patients with COVID-19 infections in North Shanghai, China [2] / Liang et al. (Feb 28, 2020), report on 457 patients with lab-confirmed COVID-19 identified from 7 studies[3]
Fever / 98% / 82.9% / 89%
Cough / 85% / 62.9% / 63%
Fatigue or weakness / 44% / 17.1% / 51%
Headache / 8% / Muscle soreness 6.7% / 8%
Diarrhea / 3% / 8.6% / 7%
Several additional reports underline the potential seriousness of a COVID-19 infection, including damage to lung tissue that has become characteristic to COVID-19. Shi et al. (Feb 24, 2020) describe this damage:
“COVID-19 pneumonia manifests with chest CT imaging abnormalities, even in asymptomatic patients, with rapid evolution from focal unilateral to diffuse bilateral ground-glass opacities that progressed or co-existed with consolidations within 1-3 weeks.”[4]
The Chinese Centers for Disease Control and Prevention (Chinese CDC) reported recently that approximately 20% of COVID-19 cases are classified as severe or critical.[5] COVID-19 infections may result in life-threatening conditions including acute respiratory distress syndrome, acute kidney injury, cardiac injury, and liver dysfunction (Table 2) and may require hospitalization, intensive care, intubation, or other significant life-saving interventions. In some cases COVID-19 may lead to death; the Chinese CDC reported that 2.3% of confirmed COVID-19 cases died.[6] The World Health Organization’s reports indicate that 3.4% of reported cases have died.[7] There is currently no cure, only supportive treatment, and no vaccine.
Table 2: Clinical Outcomes of COVID-19 Reported in the Scientific Literature
Clinical progression/outcome / Yang et al. (Feb 24, 2020), report on 52 critically ill patients with COVID-19 who were admitted to an intensive care unit (ICU) in Wuhan, China[8] / Liang et al. (Feb 28, 2020), report on 457 patients with lab-confirmed COVID-19 identified from 7 studies[9]
Acute respiratory distress syndrome / 67% / 12%
Acute kidney injury / 29% / 2%
Cardiac injury / 23% / 3%
Liver dysfunction / 29% / -
Death / 61.5% at 28 days / 8%
[1] Huang et al. (Feb 15-21 2020), “Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China.” The Lancet, 395(10223): 497-506
[2] Wang, Changhui, et al. (Feb 20, 2020), “The Epidemiologic and Clinical Features of Suspected and Confirmed Cases of Imported 2019 Novel Coronavirus Pneumonia in North Shanghai, China.” Preprints with The Lancet, published online at https://papers.ssrn.com/sol3/papers.cfm ... id=3541125.
[3] Liang, Bo et al. (Feb 28, 2020), “Clinical Characteristics of 457 Cases with Coronavirus Disease 2019.” Preprints with The Lancet, published online at https://papers.ssrn.com/sol3/papers.cfm ... id=3543581.
[4] Shi, Heshui et al. (Feb 24, 2020), “Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study.” The Lancet Infectious Diseases, published online, https://www.thelancet.com/journals/lani ... 73-3099(20)30086-4/fulltext.
[5] Wu, Zunyou and Jennifer M. McGoogan (Feb 24, 2020), “Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention.” JAMA, published online at https://jamanetwork.com/journals/jama/f ... le/2762130.
[6] Wu, Zunyou and Jennifer M. McGoogan (Feb 24, 2020).
[7] The World Health Organization’s Situation Report from March 4, 2020 indicates that 2,984 deaths have been reported in China and 214 deaths have been reported outside of China for a total of 3,198 deaths. 3,198 deaths ÷ 93,090 total cases = 3.4%. World Health Organization (March 4, 2020), “Coronavirus disease 2019 (COVID-19), Situation Report-44.” Online at https://www.who.int/docs/default-source ... 783b4c9d_6.
[8] Yang, Xiaobo et al. (Feb 24, 2020), “Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study.” The Lancet Respiratory Medicine, published online, https://www.thelancet.com/journals/lanr ... 13-2600(20)30079-5/fulltext.
[9] Liang, Bo et al. (Feb 28, 2020).
Transmission
What is known:
The virus is spread through human to human transmission. Asymptomatic cases are occurring and can be infectious. Two studies indicate that the most infectious period may actually be the first four days or so after exposure. Researchers found very high levels of the virus in upper respiratory tract samples before clinical symptoms occurred.[1,2]
What is unknown:
All modes of transmission for COVID-19 have yet to be established.
However, current epidemiological evidence supports aerosol transmission of COVID-19. Aerosols, particles suspended in air, can be transmitted by an infected person through breathing, talking, coughing, and sneezing.[3] They can also be generated during medical procedures such as intubation and bronchoscopy. Particles vary in size; larger aerosol particles can remain suspended in the air for several minutes, while smaller or lighter ones can linger in the air for hours and travel through the room and ventilation systems. Perfume spray demonstrates the extent of aerosol distribution as it can be smelled from a distance for quite some time as the particles disperse throughout the room.
Similar to SARS (severe acute respiratory syndrome), researchers have found that SARS-CoV-2, the virus that causes COVID-19, can survive and stay infectious in aerosols for at least 3 hours.[4] SARS-CoV-2 can also survive on surfaces for an extended period of time. For example, genetic material from SARS-CoV-2 was detected on a number of surfaces in the Diamond Princess cruise cabins of both symptomatic and asymptomatic infected passengers 17 days after they vacated.[5] Asymptomatic virus shedding and viability in the air and on surfaces may explain the rapid person-to-person transmission. As such, all contact and airborne precautions must be maintained to protect healthcare workers.
[1] Woelfel, Roman et al. Clinical Presentation and Virological Assessment of Hospitalized Cases Of Coronavirus Disease 2019 In A Travel-Associated Transmission Cluster. MedRxiv, Cold Spring Harbor Laboratory Press, 2020. https://doi.org/10.1101/2020.03.05.20030502
[2] Nishiura, Hiroshi, et al. Serial Interval of Novel Coronavirus (COVID-19) Infections. International Journal of Infectious Diseases, Elsevier, 2020. https://doi.org/10.1016/j.ijid.2020.02.060
[3] Jones, R.M. and L.M. Brosseau, Aerosol transmission of infectious disease. Journal of Occupational and Environmental Medicine, 2015. 57(5): p. 501-8.
[4] N van Doremalen, et al. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. The New England Journal of Medicine, 2020. DOI: 10.1056/NEJMc2004973.
[5] Moriarty, et al. Public Health Responses to COVID-19 Outbreaks on Cruise Ships — Worldwide, February–March 2020. MMWR Morb Mortal Wkly Rep. DOI: http://dx.doi.org/10.15585/mmwr.mm6912e3
Additional Resources
The situation is evolving rapidly. Please see the links below for the most up-to-date information.
World Health Organization (WHO)’s Dashboard
https://experience.arcgis.com/experienc ... ee1b9125cd
Bibliography
Airborne precautions are needed for COVID-19.
Bourouiba, Lydia, “Turbulent Gas Clouds and Respiratory Pathogen Emissions: Potential Implications for Reducing Transmission of COVID-19,” JAMA, March 26, 2020, https://jamanetwork.com/journals/jama/f ... le/2763852.
Summary:
• This paper reported on what is known about disease transmission via respiratory droplets created by human exhalations, sneezes, and coughs.
• Droplet transmission was originally defined in 1897, large and small droplets defined in 1930s. This model of infectious disease transmission hasn’t been updated since. And yet, the CDC and WHO maintain use of this paradigm despite more recent research.
• More recent research over the past few decades performed with instrumentation that better measures particle sizes and movement has determined that human exhalations, coughs, and sneezes (the things that supposedly create large droplets under old model) are actually made of multiphase turbulent gas clouds (a puff) that entrains ambient air and traps and carries clusters of particles of a wide range of sizes.
• This includes viral particles in people who are sick.
• Pathogen-carrying gas clouds emitted when people breath, cough, and sneeze can travel up to 23-27 feet.
Patients infected with SARS-CoV-2 produce viral particles that can be aerosolized when they breath, cough, sneeze, etc.
Wolfel, Roman, et al., “Virological assessment of hospitalized patients with COVID-2019,” Nature, April 1, 2020, published online at https://www.nature.com/articles/s41586-020-2196-x.
Summary:
• This study examined viral loads and isolates for patients hospitalized with COVID-19. The majority of patients in this study presented with upper respiratory tract symptoms. Viral loads from upper respiratory tract samples were extremely high (more than 1000 times higher than SARS). Live virus was isolated from upper respiratory tract tissues.
• Michael Osterholm, PhD, MPH, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, said, “The findings [of this study] confirm that COVID-19 is spread simply through breathing, even without coughing… They also challenge the idea that contact with contaminated surfaces is a primary means of spread,” (emphasis added). http://www.cidrap.umn.edu/news-perspect ... 19-viruses.
Leung, Nancy H. L. et al. “ Respiratory virus shedding in exhaled breath and efficacy of face masks,” Nature Medicine, April 3, 2020, https://www.nature.com/articles/s41591-020-0843-2
Summary:
This study examined viral presence and load in exhaled breath of patients with lab-confirmed influenza, seasonal coronaviruses, or rhinovirus.
• Found viral presence in exhaled breath, even without cough, for all types of viruses in both droplet (>5 micron) and aerosol (<5 micron) particles.
SARS-CoV-2 virus can survive in the environment, including in the air.
Doremalen et al., “Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1,” New England Journal of Medicine, April 16, 2020, https://www.nejm.org/doi/full/10.1056/N ... tured_home.
Summary:
• This study examined how long SARS-CoV-2 can survive in aerosols suspended in the air and on surfaces of different types (metal, plastic, cardboard).
• They found that SARS-CoV-2 can survive up to three hours in aerosols, four hours on copper, 24 hours on cardboard, 2-3 days on plastic and stainless steel.
• The authors conclude, “Our results indicate that aerosol and fomite transmission of [SARs-CoV-2] is plausible, as the virus can remain viable in aerosols for multiple hours and on surfaces up to days.” This study was conducted by NIH and CDC scientists in addition to UCLA and Princeton.
Chin, Alex W H et al. “Stability of SARS-CoV-2 in different environmental conditions,” The Lancet Microbe, April 2, 2020, https://www.sciencedirect.com/science/a ... via%3Dihub.
Summary:
• This study examined the ability of SARS-CoV-2 to survive outside the human body in different environmental conditions.
• They found that SARS-CoV-2 can survive outside the human body for up to 14 days at 39 degrees Fahrenheit, 7 days at 72 degrees Fahrenheit and remains infectious in both situations.
• They found that SARS-CoV-2 can survive on different surfaces:
o Printing and tissue papers- up to 3 hours
o Wood and cloth- up to 2 days
o Glass and banknote- up to 4 days
o Stainless steel and plastic- up to 7 days
o Surgical mask- detectable level of infectious virus found after 7 days on outer layer of mask
• They also tested the impact of different disinfectants, used at working concentrations, to successfully inactivate SARS-CoV-2:
o Household bleach (1:49)
o Household bleach (1:99)
o Ethanol (70%)
o Povidone-iodine (7.5%)
o Chloroxylenol (0.05%)
o Chlorhexidine (0.05%)
o Benzalkonium chloride (0.1%)
Fears, Alyssa C. et al. “Comparative dynamic aerosol efficiencies of three emergent coronaviruses and the unusual persistence of SARS-CoV-2 in aerosol suspensions,” medxRiv, April 18, 2020, https://www.medrxiv.org/content/10.1101 ... 20063784v1
Summary:
• This study looked at the viability of SARS-CoV-2 in suspended aerosols and found that SARS-CoV-2 remained infectious after 16 hours suspended in aerosols. This further reinforces airborne/aerosol transmission of SARS-2.
• The authors state: “Our approach of quantitative measurement of infectivity of viral airborne efficiency complemented by qualitative assessment of virion morphology leads us to conclude that SARS-CoV-2 is viable as an airborne pathogen.”
Environmental contamination
Guo, Zhen-Dong et al., “Aerosol and Surface Distribution of Severe Acute Respiratory Syndrome Coronavirus 2 in Hospital Wards, Wuhan, China, 2020,” Emerging Infectious Diseases, April 10, https://wwwnc.cdc.gov/eid/article/26/7/20-0885_article.
Summary:
• This study looked at environmental contamination in an ICU and a general ward in hospital in China where patients with COVID-19 were placed.
• They found SARS-CoV-2 on many surfaces in patient rooms and on units, including doorknobs, bedrails, patient masks, computer mouse, keyboards, etc.
• Many positive results on floors not just in patient room but throughout the unit. 50% of the samples from the soles of healthcare workers’ shoes were positive.
• They also measured SARS-CoV-2 in air samples and found several air samples positive in addition to finding that the samples from the air outlets were positive for virus.
• Underlines nurses’ need for PPE!
Santarpia, Joshua L et al., “Transmission Potential of SARS-CoV-2 in Viral Shedding Observed at the University of Nebraska Medical Center,” medRxiv (pre-print), March 26, 2020, https://www.medrxiv.org/content/10.1101 ... 20039446v2.
Summary:
• This study looked at the presence of virus in air samples taken in patient rooms in addition to environmental samples.
• SARS-CoV-2 was found in a majority of air samples taken at greater than 6 ft from patient.
• SARS-CoV-2 was found in a majority of hallway air samples.
• SARS-CoV-2 was found in the air samplers worn by sampling personnel even when the patients did not cough.
Chia, Po Ying et al. “ Detection of Air and Surface Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in Hospital Rooms of Infected Patients” medRxiv April 9, 2020, https://www.medrxiv.org/content/10.1101 ... 1.full.pdf
Summary:
• This study examined surface and air contamination in airborne infection isolation rooms of patients with confirmed COVID-19 infections in Singapore.
• They found that 56.7% of the rooms had at least one environmental surface contaminated, with 18.5% of the toilet seats and toilet flush button being contaminated.
• High touch surface contamination was shown in ten (66.7%) out of 15 patients in the first week of illness, and three (20%) beyond the first week of illness (p = 0.010).
• Air sampling of two COVID-19 patients (both day 5 of symptoms) detected SARS-CoV-2 PCR positive particles of sizes >4 µm and 1-4 µm. In a single subject at day 9 of symptoms, no SARS-CoV-2 PCR-positive particles were detected.
Protective PPE, including at minimum N95 respirators, gowns/coveralls, eye protection, and gloves, is important to protect nurses and other healthcare workers from exposure to SARS-CoV-2.
Cheng, C.C. et al., (March 5, 2020), “Escalating infection control response to the rapidly evolving epidemiology of the Coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong.” Infection Control and Hospital Epidemiology, March 2020, p 1-24 https://www.cambridge.org/core/journals ... DC747EB6EC
Summary:
• Hong Kong has more effectively contained the outbreak of COVID-19 than many other countries. This study reports a description of infection control measures adopted during response to COVID-19 in Hong Kong.
• 42 of 1275 patients evaluated were identified as having COVID-19 in first 42 days of the outbreak.
• 11 of 413 (2.7%) healthcare workers caring for these patients had unprotected exposure requiring a 14-day quarantine.
• No healthcare workers were infected, no nosocomial transmission observed. Environmental surveillance of viral particles conducted- in breathing zone of patient, wipe samples from surfaces in patient rooms.
• Infection control measures implemented include:
o 36 patients immediately isolated upon admission in AIIRs, 6 in non-AIIR
o Standard, contact, droplets, and airborne precautions for suspected or confirmed cases
o Stepped up use of PPE during aerosol generating procedures
o Surgical masks worn by all HCWs, patients, and visitors in clinical areas implemented since day 5
o Promotion of hand hygiene by HCWs and patients
Wang, Xinghuan et al. “Association between 2019-nCoV transmission and N95 respirator use” J Hospital Infection, March 3, 2020, https://www.journalofhospitalinfection. ... 95-6701(20)30097-9/fulltext
Summary:
• This study examined the infection rate in two groups of departments.
o Three departments were in the “mask group” because they utilized N95 respirators and also frequently performed hand hygiene (respiratory, ICU, and Infectious Disease).
o Three departments were in the “non-mask group” because early in the outbreak they hadn’t implemented precautions- staff did not wear masks and disinfected and cleaned hands “occasionally.”
• There were significantly more confirmed or probable COVID-19 patients cared for in the departments in the “mask group,” meaning workers in those units had significantly more exposure than the “non-mask group.”
• “Mask group” reported statistically significantly fewer infections than the “non-mask group.”
o 0 out of 278 staff in “mask group” were infected
o 10 out of 213 staff in “no mask group” were infected
o Difference was found to be statistically significant
• Found similar results in two other hospitals- staff wearing N95s and frequently conducting hand hygiene were not infected
Chen, Weiyun et al “ To Protect Healthcare Workers Better, To Save More Lives,” Anesthesia & Analgesia, March 30, 2020, https://journals.lww.com/anesthesia-ana ... 95724.aspx.
Summary:
• This study reported on healthcare worker protections implemented in China during three phases.
• First stage- this was an unknown disease and healthcare workers were not protected. At this time, the infection rate ranged from 3.5% to 29% among healthcare workers in different hospitals in the epicenter of Wuhan according to previous reports, when the initial source of the novel coronavirus still remained unknown.
• Second stage- inadequate protection for healthcare workers due to supply shortages. During this period of time, the number of confirmed cases in China was still increasing rapidly. By February 11, 2020, a total of 1,716 health care workers were confirmed with COVID-19, including five deaths.
• Third stage- disease severity acknowledged and full protection of healthcare workers. “The highest level of precaution, so called “full precaution,” is mandatory for high-risk exposure, a disposable surgical cap, test-fit N95 masks or respirators, gloves, goggles or face shield, gown and fluid-resistant shoe covers. We would like to point out that the key element of full precaution is the complete coverage of the head and facial skin…” No healthcare worker infections reported in this third period.
Employers Must Prepare to Keep You Safe
In situations like this one where knowledge is lacking about a health threat, there is often debate about what actions to take and when. Too often healthcare employers prioritize saving money over safe care and wait to act— this is unacceptable.
Hospitals and other healthcare employers have the duty and responsibility to prepare ahead of time to protect staff and patients. And in situations like the current outbreak, to follow the precautionary principle. The precautionary principle states that we should not wait until we know for sure that something is harmful before we take action to protect people’s health. Full precautions mean anticipatory or protective action must be taken to prevent possible or further harm.
Following the precautionary principle is necessary to protecting nurses and other healthcare workers from the hazard posed by an emerging infectious disease like COVID-19. Nurses and other healthcare workers have a fundamental right to a safe and healthful workplace and infectious diseases should be no exception. Full protection of healthcare workers is a fundamental and necessary part of limiting the spread of viruses.
Of employers, NNU is asking the following:
1. Employers shall implement plans and protocols in response to COVID-19 based on the precautionary principle, which holds that lacking scientific consensus that a proposed action, policy, or act is not harmful – particularly if that harm has the potential to be catastrophic – such action, policy, or act should not be implemented and the maximum safeguards should be pursued.
2. Employers shall clearly communicate with all RNs/health care workers, including notifying nurses when there is a possible or confirmed COVID-19 case.
3. Employers shall provide education and training for all RNs/health care workers, including on protective gear, donning and doffing, and all other protocols relating to COVID-19.
4. Employers shall provide the highest level of protection, including functioning negative pressure rooms and personal protective equipment for nurses providing care to possible and confirmed COVID-19 cases. Employers must ensure negative pressure rooms remain functional at all times during use. Highest level of PPE must include PAPR (powered air-purifying respirator), coveralls meeting ASTM (American Standard for Testing and Materials) standard, gloves, temporary scrubs, and other protections.
5. Employers shall plan for surge of patients with possible or confirmed COVID-19, including plans to isolate, cohort, and to provide safe staffing.
6. Employers shall conduct a thorough investigation after a COVID patient is identified to ensure all staff and individuals who were exposed are identified and notified. Any nurse/health care worker who is exposed to COVID-19 will be placed on precautionary leave for at least 14 days and will maintain pay and other benefits during the full length of that leave.
Documents:
• Learn more about NNU's nurse and patient protection recommendations (PDF)
• Download our NNU/National flier on protections at work for COVID-19 (PDF)
• Download our CNA/California flier on protections at work for COVID-19 (PDF)
________________________________________
Nurses' Statements
• March 24, 2020 - Statement by National Nurses United Nurses About Making Homemade Facemasks for Health Care Workers
• March 23, 2020 - Nurses Send Petition to Congress Demanding Immediate Protections During COVID-19 Outbreak
• March 23, 2020 - Union Workers in the Building Trades Donate Masks to Nurses Amidst Government Inaction
• March 21, 2020 - Nurses: California Needs to Do More on Protective Gear
• March 20, 2020 - Updated COVID-19 survey of registered nurses shows little improvement and worsening availability of personal protective equipment
• March 16, 2020 - Nurses: Time to sharply ramp up health care capacity for COVID-19
• March 14, 2020 - Nurses Say Eastern Maine Medical Center Has Addressed Many of Their Concerns Over COVID-19 Safety Preparations
• March 14, 2020 - Veterans Health Administration unions decry management’s failure to involve them in COVID-19 preparations, call to work together
• March 13, 2020 - National Nurses United statement on today’s Trump administration press conference
• March 11, 2020 - Recording of National Nurses United COVID-19 Update Call Available on Website
• March 5, 2020 - Survey of Nation’s Frontline Registered Nurses Shows Hospitals Unprepared For COVID-19
• March 5, 2020 - Statement by a quarantined nurse from a northern California Kaiser facility
• March 2, 2020 - National Nurses United Urges Administration, Congress to Protect Health Care Workers and Fully Fund Coronavirus Response
• March 2, 2020 - General Statement - California Nurses Association/National Nurses United Monitoring Coronavirus
• Feb 28, 2020 - Nation’s hospitals unprepared for COVID-19
________________________________________
Letters to Officials
• April 3, 2020 - Letter to Centers for Disease Control and Prevention on N95 Decontamination as Unsafe Practice
• March 17, 2020 - Petition to Congress for Proper Nurses Protection During COVID-19
• March 11, 2020 - Letter to Sacramento County Department of Health Services on 14 Day Quarantine
• March 11, 2020 - Letter to California Department of Public Health
• March 11, 2020 - Letter to Committee on Homeland Security
• March 6, 2020 - Labor's Response to CDC Incident Manager for Coronavirus
• March 4, 2020 - Letter to CDC Incident Manager for Coronavirus
• March 4, 2020 - Letter to Secretary of Labor and Federal OSHA
• March 2, 2020 - Letter to Office of the Vice-President, Coronavirus Response Coordinator, Members of United States Senate and House of Representatives
• Feb 21, 2020 - Letter to Chief of Cal/OSHA
• Feb 19, 2020 - Letter to National Center for Immunization and Respiratory Disease
• Feb 19, 2020 - Letter to California Department of Public Health
• Jan 30, 2020 - Letter to the World Health Organization